To brace or not to brace? Bracing for neuromuscular conditions
There is no doubt about it: braces are a pain. Sometimes they are a literal pain, causing pain for your child. And sometimes they are a more figurative pain in the rear end—difficult to deal with, difficult to get on and off, difficult to force onto your child.
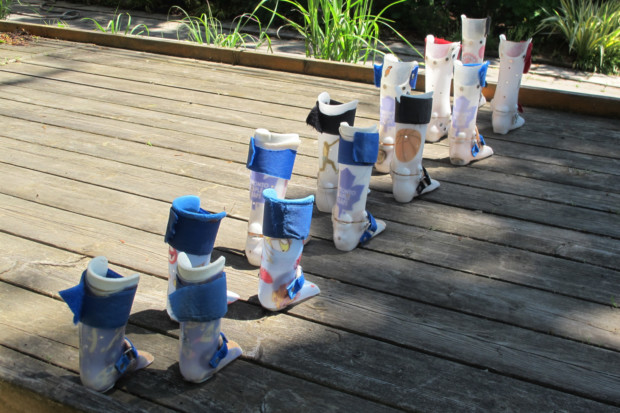
These braces were made for walking. Disabled Families
Susan Agrawal, Complex Child October 21, 2013
Despite their drawbacks, braces can also be incredibly helpful. They can help our children achieve things that otherwise would not be possible, such as standing. They can preserve a correction after surgery. And in some cases, they can prevent or even correct an orthopedic problem.
How do you know when you should brace, and when it is just not worth it? I’ll try to answer that question, or at least provide you with the right questions to think about, in the sections below.
| Reasons for Bracing |
There are four general reasons for bracing:
- Post-correction bracing, such as bracing after surgery
- Bracing for function, such as bracing the ankles to allow standing or walking
- Preventative bracing, such as bracing to prevent skin breakdown or a contracture
- Corrective bracing, such as serial casting to straighten a wrist or ankle

Bracing and casting after hip surgery. Complex Child
The first type of bracing, post-correction bracing, is virtually always required and not even remotely controversial. This type of bracing follows any corrective procedure, such as surgery, botox or phenol injections, or serial casting.
Once the correction has taken place, bracing is necessary to maintain the changes created by the surgery or other method of correction.
In many cases, bracing is temporary and will only last for a few weeks or months.
In some cases, however, bracing may be required long term. Even if post-correction bracing is uncomfortable for your child, it is worthwhile to maintain correction.
Bracing for function is also not particularly controversial. If a brace can be used to improve a child’s ability, it should by all means be used, as long as it is comfortable for the child. Examples of bracing for function include the use of a TLSO or other back brace to assist with sitting and standing; ankle or knee orthoses to help with standing or walking; wrist, hand, or finger bracing to assist with fine motor skills; or applying a neck collar to assist in using a head switch.
Of course, there are instances when the brace itself is so uncomfortable that its drawbacks are worse than its benefits. In this case, a different type or style of brace may be tried, or bracing may be discontinued. Most of the time, a different type of brace can solve the problem. Always ensure that braces are designed by, constructed, or selected by a certified orthotist with pediatric experience to maximize success.

Thoracic Lumbar Sacral Orthosis, TLSO. Complex Child
Preventative bracing is far more controversial. Part of the reason it is controversial is because it often does not work, especially for children with severe neuromuscular disorders. Sometimes it may delay a complication, and other times it may minimize a complication. For example, many children with severe cerebral palsy wear TLSOs or other back braces to prevent scoliosis. The evidence in this population shows that scoliosis tends to develop no matter what the intervention. Surgery is often needed, whether a child is braced or not.
Bracing may delay the surgery or minimize the scoliosis, but the scoliosis will likely develop even with bracing. In this situation, it is important to evaluate the potential benefits and see if the bracing will cause quality of life issues.
If a brace is well-tolerated and seems to be beneficial, definitely continue using it. But if the brace is causing discomfort, interfering with sleep, or otherwise having a negative effect, and the likelihood of any benefit is low, it may be better to stop bracing. Children often tolerate certain types of preventative braces, such as AFOs (ankle foot orthotic) or hand/finger splints, better than other types of braces.
Corrective bracing can be very beneficial, but only in certain instances. Deformities that are congenital, such as clubfoot, respond very well to bracing or serial casting, which consists of a series of casts that gradually change the position of a limb over time. Corrective bracing may also work well for children with neuromuscular conditions that are mild to moderate.

AFOs help this child sit and stand properly. Complex Child
For these children, corrective bracing may allow a new or improved ability, such as walking with a walker.
However, the child must be able to maintain the correction through daily use. Many children with severe cerebral palsy simply are unable to maintain the correction over time, as high muscle tone will continue to exacerbate the problem. Corrective bracing is most useful in correcting limb-related issues, such as ankle, knee, wrist, or elbow problems. It may also help with neck problems like torticollis. It is less successful in fixing trunk problems, such as scoliosis or kyphosis.
Of course, a brace may serve multiple purposes. AFOs may allow for standing while also preventing contractures from developing. Wrist braces may correct contractures while also allowing greater ability to use a pointer.
| Bracing Conundrums |
When deciding whether or not to brace, these are a few of things you might want to think about:
| General Use |
Ask yourself the following questions:
- Does the brace improve my child’s function?
- Is this brace necessary to prevent future pain and suffering?
- Are we seeing any benefit from this brace?
- Does this brace cause my child discomfort?
- Is the brace so difficult to use that it is not being worn?
- Does the brace interfere with my child’s sleep or quality of life?
- Does the brace improve positioning?
- Does the brace eliminate current pain, skin breakdown, or other discomfort?
| Goals |
It is important to know the purpose of a brace. Will it prevent future problems? Is it being used for a functional purpose? Will it improve standing or walking?
Knowing the purpose of the brace, and how important that purpose is in your overall goals for your child, will help you determine the overall value of bracing.
| Prognosis |
If your child’s prognosis is very poor, you most likely will want to focus on comfort. For many children, this will mean foregoing certain types of bracing, while for others, bracing might be used to minimize or eliminate pain. Quality of life is key for these children.
On the other hand, if your child is expected to live well into adulthood, you may want to put extra effort into preventative bracing in order to minimize pain and surgery in the future.
| When Braces are Used |
Some children wear braces 24 hours a day, while others only use them for certain functional activities. For a child with severe neuromuscular issues who is unlikely to receive much orthopedic benefit from bracing, you may only want to use braces during certain activities when the brace improves function.
Other children may need to wear braces more often to prevent contractures and future problems. In general, if braces are interfering with sleep, they should not be used, except in the short term after surgery.
| Comfort |
Some types of braces are better tolerated than others. For example, AFOs (ankle braces) tend to be well-tolerated, while back braces or wrist splints may be less comfortable. Any well-tolerated brace should be worn regularly. If a brace is uncomfortable, try a different type or style.
If it continues to be uncomfortable, consider discontinuing the brace. In some cases, medications like botox or baclofen may be equally or more effective than bracing. Custom positioning equipment may be another option for some children.
| The Key: Trial and Error |
The only true way to make your decision is to give bracing a try and see what happens. If it helps and isn’t bothering your child, you are good to go.
But if it is a struggle, causes pain, or seems to have no benefit, it is just fine to say no way.
| This information is not a substitute for appropriate medical care. Please contact your child’s physicians before making any changes in your child’s care. Complex Child is for research purposes only and does not constitute medical advice. |
| Complex Child is a monthly online magazine written by parents of children with special healthcare needs and disabilities. It is intended to provide medical information, along with personal experiences, in simple language that other parents can understand. Articles are on a wide variety of topics ranging from basic information on medical conditions and treatments to advice on how to beat insurance company denials. |
| Subscribe to our monthly newsletter, which notifies you by email when a new edition is available. Also, feel free to like our Facebook page and follow our Twitter page. |
| Susan Agrawal, the editor of Complex Child, is the parent of Karuna, a child with complex medical needs who passed away 9/19/2014. Karuna was diagnosed with cerebral palsy secondary to hypoxic ischemic encephalopathy, and a progressive disorder that was likely autoimmune causing multisystem organ failure. Karuna was vent-dependent, had a GJ tube, a central line, was 100% TPN (IV nutrition) dependent, was on oxygen, and used a Foley catheter. |
| Susan holds a humanities PhD and used to serve on the faculty of a top research university in the Chicago area. She is actively involved with Feeding Tube Awareness Foundation as a content specialist and board member. In addition to her work on Complex Child, she also maintains Kids’ Waivers, a website devoted to information on Medicaid waivers for children, and helps run MFTD Waiver Families, an advocacy and support group for families in Illinois who receive home nursing. |
| She currently cares for her typically developing children Sameer and Neena. |
Source Complex Child
