Electronic health records ‘inflict enormous pain’ on doctors
Electronic health records slow doctors down and distract them from meaningful face time caring for patients.
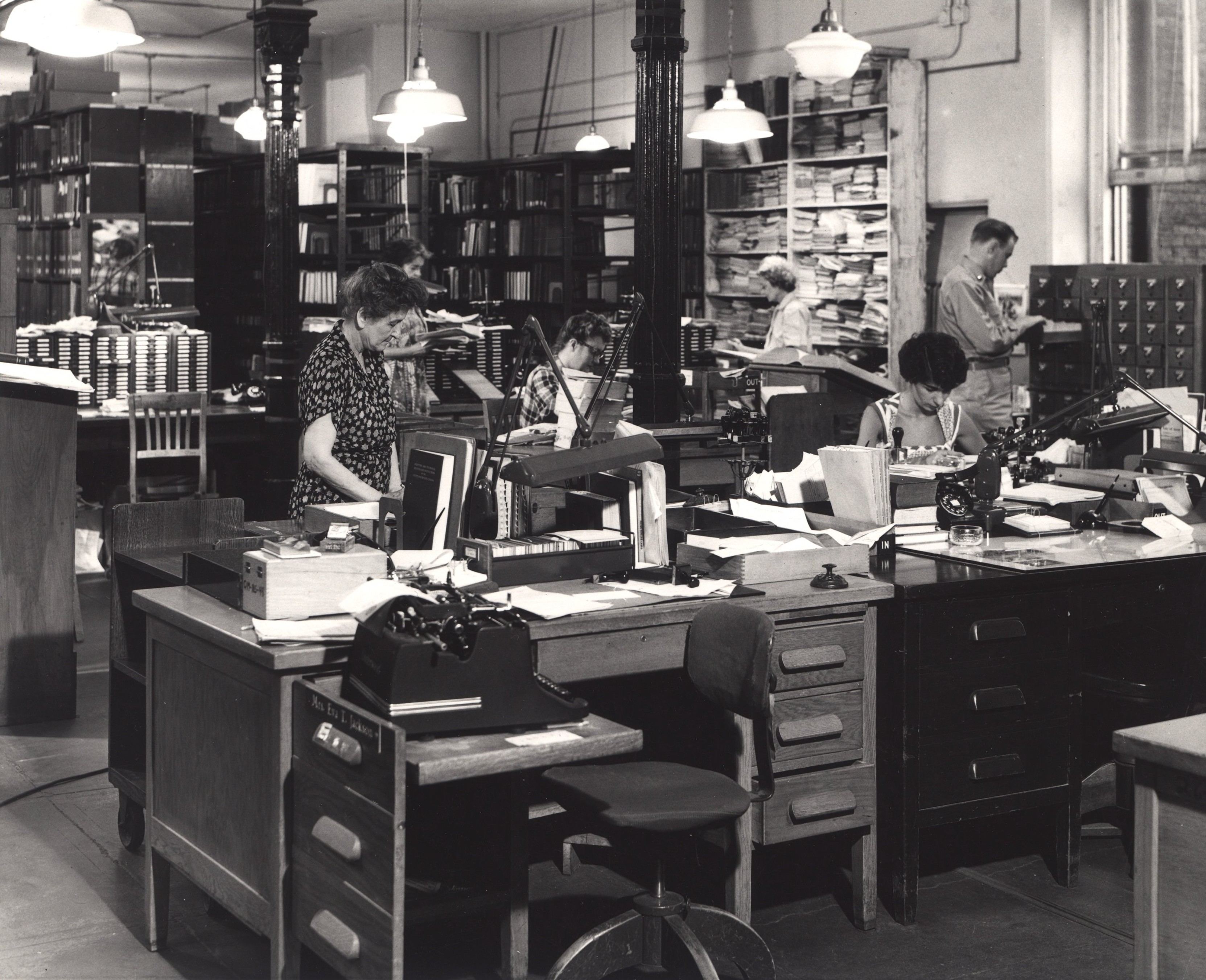
Hidden treasure. View from behind a cataloging desk, Army Medical Library, Washington, DC, ca. 1955. National Library of Medicine. Images from the History of Medicine
By Jonathan Bush, STAT September 6, 2016
That is the a sad but unsurprising finding of a time and motion study published in Tuesday’s Annals of Internal Medicine. A team of researchers determined that physicians are spending almost half of their time in the office on electronic health records (EHRs) and desk work and just 27 percent on face time with patients — which is what the vast majority of doctors went into medicine to do. Once they get home, they average another one to two hours completing EHRs.
I wish I could say I was shocked by these results. But they just add a fresh headline to old news, reinforcing what we already know too well: the more our country spends on traditional EHR software, the more time providers must spend on them, the more dissatisfied they become, the more frustrated patients feel, and the more expensive health care gets.
This is a shared problem with more than enough culpability to go around. Vendors like my company, athenahealth, and others have been required to develop EHRs that satisfy government regulations rather than the needs of providers and patients.
With limited authority and the best of intentions to oversee EHR certification and adoption, the Office of the National Coordinator for Health Information Technology continues to inflict enormous pain on our nation’s providers and care teams, turning caregivers into box-checkers and inadvertently limiting the private sector from innovating.
Motivated by more than $30 billion in incentives, vendors have lined up happily to ride the wave, building EHRs that satisfy government requirements but make it increasingly difficult and less rewarding to care for patients.
And so, we find ourselves in 2016 using the very latest stopwatches and journals to figure out just how bad our technology problem is. The very idea that we’re measuring 21st century technological performance with 19th century technology — the clipboard and stopwatch — is a nightmare of the absurd that only health care (or possibly Terry Gilliam) could conjure up.
Do you think Facebook or Amazon arms their teams with stopwatches to see how long a friend request or book order takes? They don’t. They look under the hood, constantly, to record user experience by the keystroke and they test fixes and changes in near real-time in a continuous feedback loop.
It’s time for health care to stop retreading old ground and instead embrace the kind of user-centric innovation pioneered by the likes of Amazon, Facebook, Uber, and other network-based revolutionaries. Network-enabled technology, which my company and clients run on, is still the radical exception in health care, even though it is the norm in many other industries.
While the Athenahealth EHR is far from perfect, it doesn’t require a stopwatch to measure. We can and do track exactly how much time doctors spend documenting in the exam room with a patient or after hours at home. For example, we know that women physicians work on the EHR at night more often and longer than men. This isn’t self-reported information, as in the Annals article, but is directly measured.
One of our corporate scorecard metrics (which directly affect employee bonuses) this year is to decrease the amount of time physicians spend documenting patient visits after hours. Because our EHR is delivered over a network we know exactly how much time providers and staff spend on patient care vs. administrative work, and use that data to test and drive improvements.
This type of accountability needs to become the industry norm. Key measures like after-hours EHR documentation and time spent in face-to-face patient care will help squelch health care’s technology problem, bring transparency to the most offensive solutions in the market and, more important, will chip away at care team burnout and dissatisfaction.
Improving quality while reducing costs and delighting providers and patients is the Holy Grail. We will reach it only if we reimagine the existing health care process in which we are trapped. Efforts are in the works around the country to advance price transparency. Movements are slowly taking hold around value-based reimbursement. The call to break down health care data silos has been sounded. And initiatives to boost both physician and provider engagement are taking root. But when will we declare that the software-based EHR, as we’ve known it, is dead?
I’m starting the stop watch for this declaration now.
| Jonathan Bush is CEO and president of Athenahealth, a health care technology company based in Watertown, Mass., and author of the New York Times bestseller, Where Does it Hurt? An Entrepreneur’s Guide to Fixing Health Care. |
Source STAT
| References |
Allocation of Physician Time in Ambulatory Practice: A Time and Motion Study in 4 Specialties, Christine Sinsky, MD; Lacey Colligan, MD; Ling Li, PhD; Mirela Prgomet, PhD; Sam Reynolds, MBA; Lindsey Goeders, MBA; Johanna Westbrook, PhD; Michael Tutty, PhD; and George Blike, MD. Ann Intern Med. Published online 6 September 2016 doi:10.7326/M16-0961
Also see
HIPAA turns 20: Five things you should know about your medical records STAT
Hospitals face budget woes with switch to electronic records STAT
Physicians spend nearly 50% of their time on EHR, desk work Healio
More than half of US physicians experiencing professional burnout Healio
