Wearable stomach monitor could help salvage a technology largely abandoned by gastroenterologists.

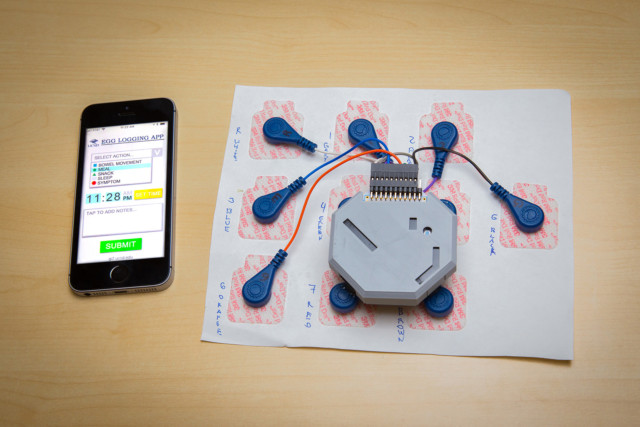
Researchers have developed a wearable system to monitor stomach activity that performs as well as current state of the art methods but can be used outside of a clinical setting. The system also comes with an app that allows patients to log their meals, sleep and other activities. UC San Diego
By Elie Dolgin, IEEE Spectrum March 30, 2018
A new wearable device that non-invasively monitors electrical activity in the stomach could help people with digestive problems determine with greater precision whether treatments or diets are working.
If clinically validated, the stomach sensor could also help revive a medical technology called electrogastrography (EGG) that once piqued gastroenterologists’ interest, but has largely fallen out of favor owing to controversy surrounding its diagnostic relevance.
“It’s promising technology,” says Thomas Abell, a gastroenterologist who routinely uses EGG at the University of Louisville but was not involved in the new study. “This might prove to be a clinically useful tool that people accept.”
EGG works much like an electrocardiogram, except instead of recording electrical activity of the heart it picks up electrical signals that travel through stomach muscles to control gastric contractions.
The method is designed to test whether so-called slow waves originating from pacemaker cells of the stomach are oscillating at a healthy 3 cycles per minute. But the signals detected by adhesive electrodes on the skin are often weak and muddied by artifacts of stomach movement.
The technique had a brief clinical heyday in the 1990s, but the world’s gastroenterologists have since largely abandoned it. “I view it as the Rodney Dangerfield of GI motility,” says Abell. “It gets no respect.” 3CPM, one of the only companies with an EGG system still on the market today, sold fewer than 10 units per year in the late-2000s, according to company CEO Mark Noar (although he notes that sales have picked up again, with 45 of the $25,000 machines purchased by customers around the world in 2017).
Todd Coleman and Armen Gharibans, bioengineers from the University of California, San Diego, set out to fix what they saw as pitfalls in the gastric gauging technology. First, they upped the number of channel recordings from the single waveform found in conventional EGGs like those sold by 3CPM to a whopping 25 data-collecting channels. They also created a smaller version with just eight channels to enable mobile recordings on the go.
The researchers next optimized the electrode placement, arranging the dime-sized cups in a grid below the sternum and over the bellybutton. And most importantly perhaps, they developed an algorithm that removes electrical noise (originating from external motion) from the true slow-wave signal associated with internal stomach muscle movements. The algorithm also weights the cleaned-up signals from each electrode to emphasize those relaying the most physiologically relevant readouts.
Coleman and Gharibans teamed up with their UCSD colleague Hayat Mousa, a pediatric gastroenterologist at Rady Children’s Hospital-San Diego, to test the device on 11 kids, aged 7 to 17, each of whom had chronic stomach problems. They affixed their “high-resolution” EGG set-up to each child, while simultaneously administering a more invasive diagnostic procedure called manometry, in which a catheter containing pressure transducers is passed through the nose or mouth to measure contractions at the base of the stomach.
As reported last week in the journal Scientific Reports, the results of the two tests were significantly correlated for each and every youngster evaluated. By comparison, conventional one-channel EGG recordings without the signal-to-noise filtering matched the manometry readings in only three of the 11 study subjects.
“That’s a notable finding,” says David Levinthal, director of the Neurogastroenterology and Motility Center at the University of Pittsburgh. “This is clearly better than what we had before.”
Still, that doesn’t necessarily make the test clinically meaningful.
For one thing, the results indicate that high-res EGG can capture about one-third of the variation in stomach contractions, as measured by manometry—which still leaves the bulk of what’s causing those contractions unexplained.
Plus, the many channels that feed into the EGG setup are mainly used to find the best signal of electrical activity, not the spatial arrangement. That may be valuable for knowing if the frequency of slow wave rhythms is faster or slower than the normal 3 cycles per minute, says Aydin Farajidavar, a biomedical engineer at New York Institute of Technology, “but it doesn’t tell us anything about the pattern distribution of slow wave propagation.”
Moreover, “the stomach is not just a tube that has this wave of contraction going from the esophagus down to the duodenum,” notes Levinthal. “It is a regionally specialized capacitance organ and a mixer and a grinder”—all activities that could be independently disrupted in various stomach diseases.
That leads some critics to dismiss the idea that EGG—even newer and improved EGG methods—will ever have diagnostic value. “Spontaneous EGG by itself has objective physiological limitations that render it unreliable, no matter what,” says Martin Mintchev, a biomedical engineer at the University of Calgary.
Levinthal, however, is keeping an open mind: “It’s worth entertaining the idea that there could be electrical signatures of different disorders,” he says.
Coleman and Gharibans hope to win over skeptics with further experimental data. Already, in collaboration with UCSD gastroenterologist David Kunkel, they’ve tested their prototype on around 25 adults with digestive disorders at the university’s Jacobs Medical Center, and found in as-yet unpublished work that the electrical signals sync with problems such as abdominal pain, heartburn, and bloating. “It actually does correlate with symptom severity,” Coleman says.
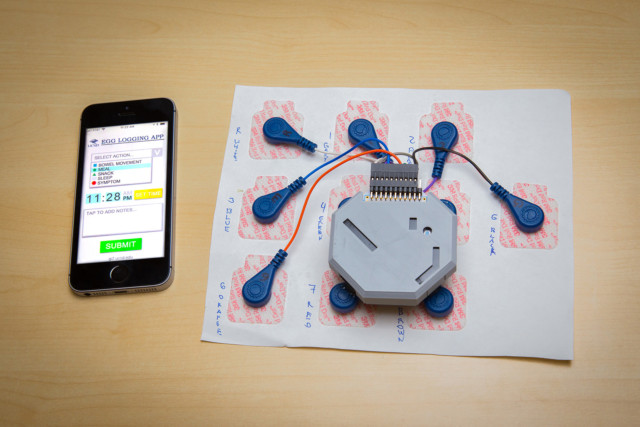
The stomach sensor syncs with an app to pair internal electrical signals with meals, bowel movements, and other gastrointestinal events. University of California San Diego
Meanwhile, as the hospital-based tests were going on, Gharibans was also hard at work developing an app for keeping tabs on meals, snacks, bowel movements, nausea, vomiting, or any other events of gastrointestinal interest. He also filled a drab-gray, 3D-printed plastic box with an accelerometer, lithium polymer battery, microSD card, and circuit board to record movement patterns and gastric electrical signals from the comfort of his home.
On eight non-consecutive days over the span of about six months, Gharibans strapped the minidisc player–sized device to his own belly for 24-hour-long recording sessions. “You don’t even really notice it too much,” he says. “As long as you don’t sleep on your stomach, it’s fine.”
Gharibans’ measurements revealed how daily activities like sleep, meals, and exercise all impacted the electrical signals in his stomach. He and Coleman now hope to get the portable device into the hands—or onto the bellies—of more patients for at-home monitoring of stomach ailments. Their vision is for people with perpetual stomach issues to wear the high-res EGG and then track in real-time, in a quantitative and objective way, whether any changes in diet or medications are bringing about gastrointestinal relief. “That’s the potential,” Coleman says.
One of the first people (other than Gharibans) to have given the device a try is Dana Lewis, founder of the Open Artificial Pancreas System project, an effort among DIYers with type 1 diabetes to create their own open-source technologies for automating blood-sugar management.
Most evenings, for the past few weeks, Lewis has taken a shower and then stuck a dozen pieces of medical adhesive to her abdomen. One is for her insulin pump, another for her glucose monitor—the two devices needed for Lewis to control her diabetes. The other 10 hold the electrodes for the UCSD team’s high-res EGG.
Lewis hopes the data she gathers about her own stomach movements following different types of meals, when matched to her blood-sugar levels, will help her improve the algorithm behind her closed-loop insulin dosing system.
“Having this picture of stomach activity and digestion will help clear away some of the noise,” she says. “Hopefully we can adapt what we’re doing to match what’s actually happening inside the body.”
| The project is a collaboration between bioengineers at UC San Diego, clinicians at Rady Children’s Hospital and the UC San Diego School of Medicine, and neuroscientists at UC Berkeley. Based upon his PhD work on this topic, Gharibans has been recognized as a Siebel Scholar, an award that recognizes exceptional students at the world’s leading graduate schools of business, computer science, and bioengineering and provides them with a financial award for their final year of studies. |
Source IEEE Spectrum
Artifact Rejection Methodology Enables Continuous, Noninvasive Measurement of Gastric Myoelectric Activity in Ambulatory Subjects, Armen A. Gharibans, Benjamin L. Smarr, David C. Kunkel, Lance J. Kriegsfeld, Hayat M. Mousa & Todd P. Coleman. Scientific Reports volume 8, Article number: 5019 (2018) doi:10.1038/s41598-018-23302-9
Also see
A wearable system monitors the stomach’s activity throughout the day in University of Calfiornia San Diego