UCSF Pectus carinatum orthosis: A pilot study
Originally presented in 1996, in memory of O&P education pioneer Howard R. Thranhardt, the annual Thranhardt Awards have become synonymous with exceptional educational information and the highest caliber research advancing the O&P field.

Josephine Rossi, O&P Almanac September 2021
This year also marked a milestone for the award and lecture series — 25 years of honoring the best and brightest minds in the profession. During the celebratory event, held during the AOPA National Assembly in Boston, the three 2021 winners presented their work to attendees in person and virtually.
Chrysta Irolla MS MSPO CPO and Emily Nelson MSE MSOP CP expounded on their study, Treatment Parameters for the UCSF Pectus Carinatum Orthosis: A Pilot Study. O&P Almanac recently spoke with the honorees about their research and what it means for the future of O&P patient care.
| Chrysta and Emily, what is pectus carinatum and how has it been treated in the past? |
Emily Nelson: Pectus carinatum is a chest wall deformity that presents as a protrusion of the sternum due to overgrowth of the costal cartilages. It is most commonly diagnosed in adolescent males during a longitudinal growth spurt.
Chrysta Irolla: Historically, pectus carinatum was treated with surgical intervention involving placement of a metal bar along the sternum. Following this procedure, there was an uncomfortable recovery period and a permanent scar. Starting in the 1990s, we saw an increase in use of orthotic interventions to correct pectus carinatum while the chest wall was still flexible, prior to skeletal maturity. There are a wide range of both off-the-shelf and custom orthotic designs that have emerged.
| What was the impetus for your study, and how is the UCSF orthosis different from prefabricated orthoses? |
Nelson: There has been research regarding orthotic treatment of pectus carinatum over the last 20-30 years; however, there is not consensus regarding the treatment parameters with these different devices. The purpose of our study is to create a detailed protocol by determining which variables have the greatest impact on successful correction of the chest wall deformity.
Irolla: From the literature and clinical experience, we found that patients often abandon use of a pectus carinatum orthosis because it is uncomfortable and excessively bulky, does not correct the chest wall deformity at a reasonable pace, does not address prominent inferior costal cartilage, and/or is hard to breathe when using. We developed the UCSF Pectus Carinatum Orthosis (UCSF-PCO) to address these specific concerns.
We made a custom design that is contoured as close to the patient’s anatomy as possible, while allowing appropriate space for ML chest expansion for breathing; includes the ability to add extensions to address the inferior costal cartilage; has a comfortable gel interface against the pectus carinatum; includes shoulder straps for appropriate suspension; and is designed to produce enough force that patients start to see correction in the first month of use.
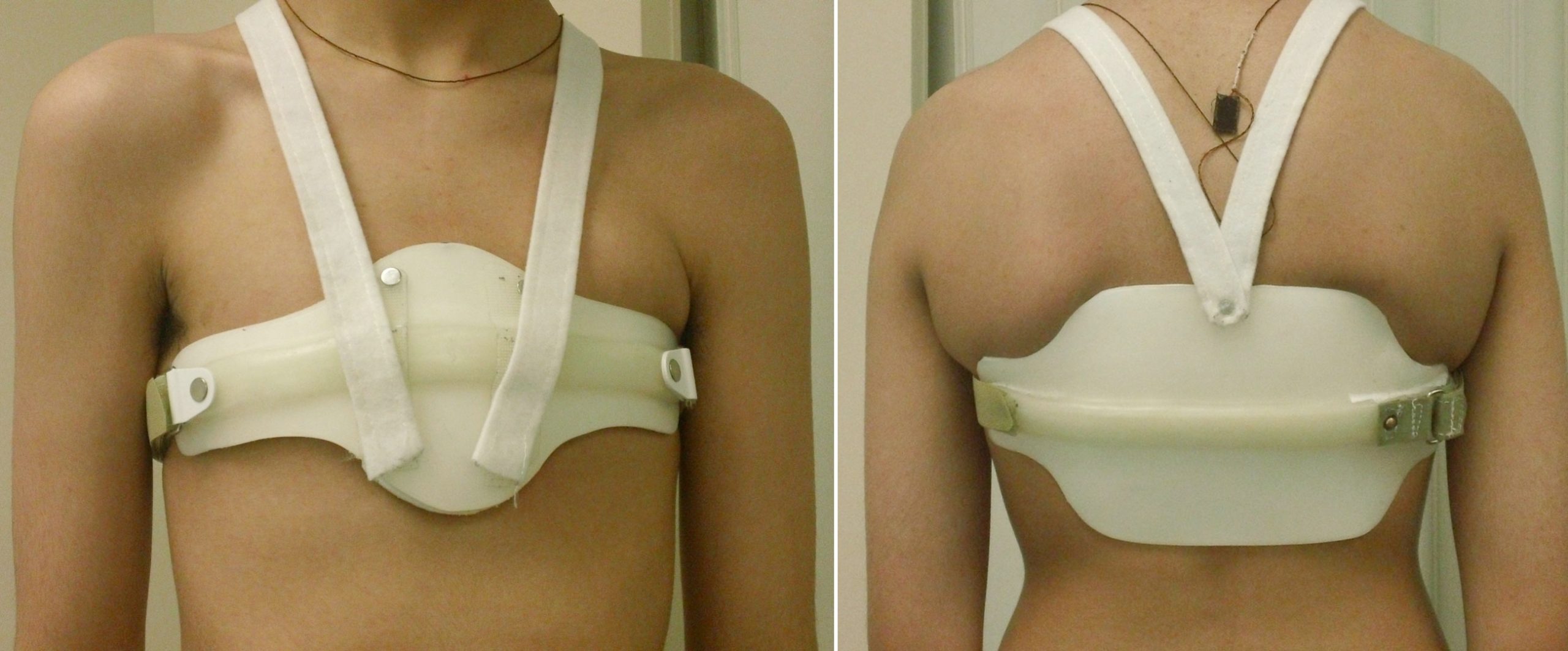
Front and back views of USCF Pectus brace
| How was your research conducted? What materials were used in the orthosis? |
Nelson: This is a longitudinal prospective clinical research study which collects both qualitative and quantitative metrics to assess success of the UCSF-PCO. We recruited a convenience sample of patients referred mostly through the UCSF chest wall deformity clinic. Inclusion criteria is 7- to 17-years-old, skeletally immature, diagnosed with flexible pectus carinatum, and recommended for conservative treatment with an orthosis.
Irolla: Each subject is provided with a custom UCSF-PCO made from 3/16″ polypropylene anterior and posterior shells with I” wide polypropylene reinforcement struts. A PediFix Visco-gel sheet pad is added to the anterior shell to provide a soft interface against the pectus carinatum. Adjustable I” Dacron backed lateral straps are used to allow for adjustability of the AP pressure and I” C-fold shoulder straps are added to help with suspension.
A Maxim Integrated Products Thermochron I-Button temperature monitor is installed in the posterior panel to track wear time. The recommended orthotic wear time is at least 18 hours per day, during the corrective phase of treatment.
At routine follow-ups, we take new measurements of the pectus carinatum size, download the data from the I-Button sensor, and use TekScan FlexiForce force sensitive resistors to measure the in-orthosis corrective pressure. Once the prominence remains reduced for a 24-hour period outside of the orthosis, the patient can transition to the maintenance phase where they only wear it at night for eight hours per day.
Nelson: Throughout treatment, we administer surveys to better understand the patient’s overall quality of life and feelings about their chest wall shape.
| What were the main findings of your research? |
Irolla: We hypothesized that subjects who were older and/or had a stiffer pectus carinatum deformity would spend more time in the corrective phase of treatment. Thus far, it does not appear there is a clear predictive relationship between age and pectus carinatum stiffness.
We also discovered that in younger subjects (7- to 13-year-olds), the pectus carinatum corrected at a meaningfully faster rate compared to the older subjects (14- to 17-year-olds).
Nelson: Younger subjects also had a reduction in pressure of treatment from delivery to final follow-up, but this was not true in older subjects.
Overall, all patients were happy with the appearance of their chest at the end of treatment, and there was no negative impact on their quality of life over the course of treatment.
| How much did social and psychological factors affect patient wear time? |
Irolla: We found that subjects in the older age group (14- to 17-year-olds) pushed to transition to maintenance phase of the treatment (eight hours per day of wear) sooner than was clinically recommended and sooner than their younger counterparts, Subjective feedback from subjects is that they did not want to wear the orthosis during high school given the increased social pressures of that environment. This earlier transition results in an increase in the length of the overall treatment time for these subjects.
| Did you encounter any limitations to your work? |
Nelson: The biggest limitation is that this treatment is conducted over a one- to two-year time frame. A number of subjects were lost to follow-up or self-discontinued their treatment outside of the clinical setting, leading to an incomplete data set. We surveyed those subjects who self-discontinued, and they mostly reported doing so because they were satisfied with the appearance of their chest wall.
| Did you discover anything surprising? |
Nelson: We expected a clear correlation between age and time to correct the pectus carinatum, and it was surprising that there was no clear trend.
| What’s next? |
Irolla: This is an ongoing study, so we are still actively recruiting patients. Our end goal is to develop a predictive model that allows clinicians to input specific physical metrics collected at an initial evaluation and outputs the transition points in pectus carinatum treatment for that specific patient. This will be a clinical tool that can better guide treatment in the future.
| Josephine Rossi is editor of O&P Almanac. Reach her at jrossi@content-communicators.com |
Source O&P Almanac
☞ Patient-reported efficacy of the UCSF custom Pectus carinatum orthosis
☞ Pectus carinatum causes, symptoms and treatment
