Gait and balance dysfunction in older adults: Challenges and interventions
Falls are a significant—yet preventable—health issue among older adults. Each year, 3 million older Americans over the age of 65 are treated in emergency departments for fall-related injuries which often result in disability, loss of independence, reduced quality of life, and death.
By Aisha Cobbs PhD, Lower Extremity Review February 2019
The number of falls is expected to rise as Americans live longer and the number of older adults continues to grow at an unprecedented rate.
If falls are preventable, why are they the leading cause of fatal and non-fatal injuries in the elderly?
The answer may be poor communication: physicians don’t ask, and patients don’t tell.
Current fall prevention guidelines recommend that physicians inquire at least annually about falls and evaluate all patients over the age of 65 for fall risk. “Most primary care physicians are good about doing diabetic foot checks, but assessing patients for fall risk is usually an afterthought,” said Robert Eckles, DPM, MPH, Dean of Clinical and Graduate Medical Education at New York College of Podiatric Medicine.
Less than half of all seniors who fall tell their doctor, so it is critical that physicians initiate the conversation. Otherwise, gait or balance dysfunctions in at-risk individuals can go undetected.
| Causes of Gait and Balance Dysfunction |
Older adults are falling for several reasons, including poor posture and loss of core strength due to lack of physical activity explained Courtney Johnson, PT, DPT, a physical therapist at Physio in Dunwoody, Georgia.
Joint deterioration and muscle weakness in the lower extremities can also cause individuals to drag their feet when they walk.
| Normal aging |
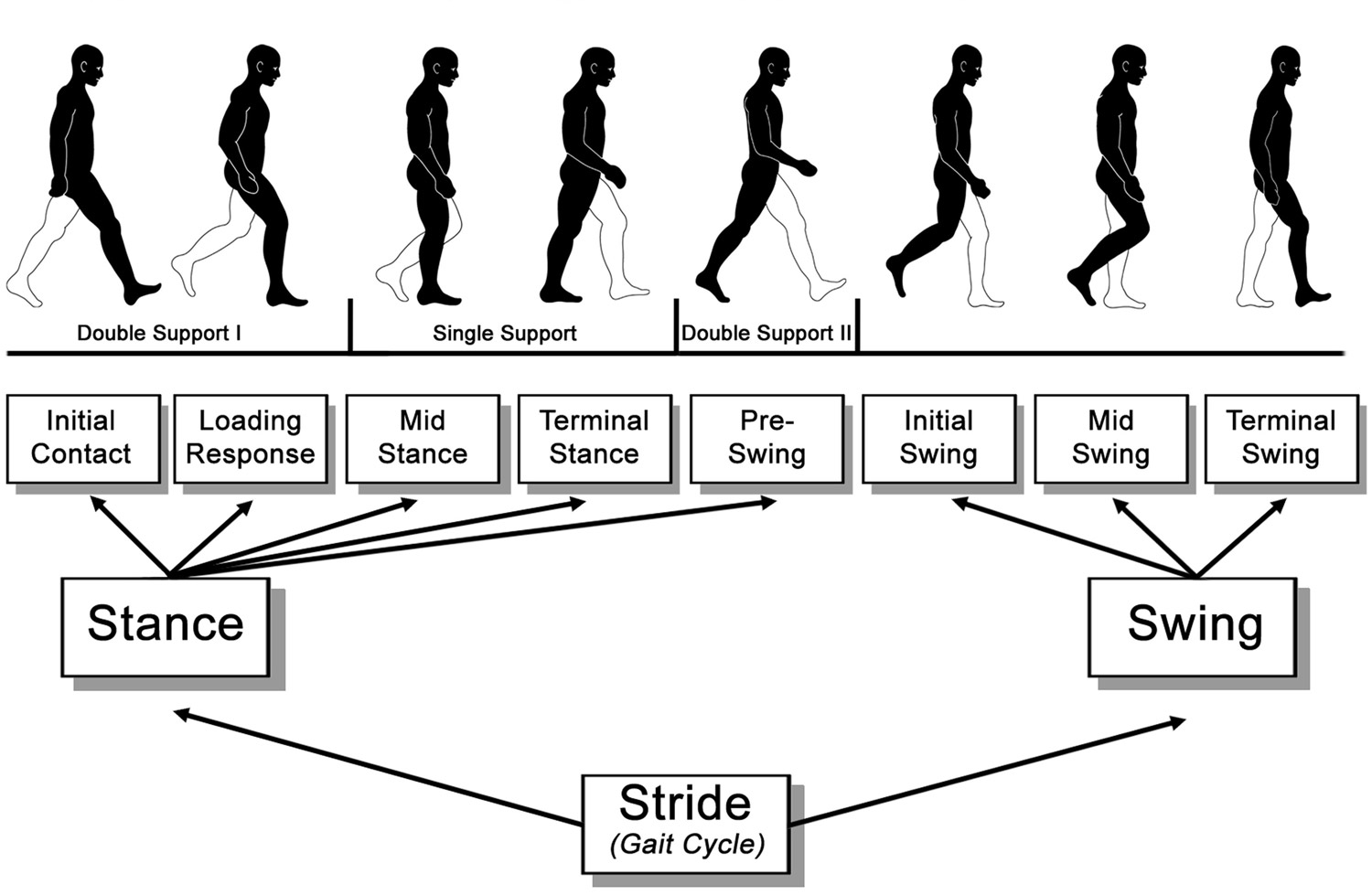
Although most abnormal gait and postural changes related to fall risk are due to underlying medical conditions, there are some gait and balance changes that are associated with normal aging. For example, healthy adults in their 70s typically have a 10% to 20% reduction in gait velocity and stride length, compared to healthy 20-year-olds.
With age, most adults also display increased stance width, increased time spent with both feet on the ground, a hunched posture, and less force during push off. Presumably, these changes help to stabilize the gait in older people.
| Pain |
Foot pain can result from neuropathy or poorly fitting footwear. Individuals with foot pain typically display decreased stride length, changes in base of gait, increased sway, increased postural stiffness, and aversion tactics—all of which significantly increase fall risk.
| Ill-fitting footwear |
Nearly 33% of adults go barefoot or wear slippers inside the house. For older adults, shoes with stiff outsoles or athletic shoes are the best for performing daily activities on a variety of surfaces. When selecting footwear, it is important that people consider that foot size changes throughout adulthood, but many people do not get their feet sized regularly.
Indeed, a 2018 systematic search and narrative review of the literature reported one survey of older adults that found that 26% of men and 47% of women had not had footwear size measured in more than 5 years. Poorly fitting shoes can cause foot pain by restricting movements or by producing friction blisters.
| Prescription medications |
Many of the drugs prescribed to older adults can impair balance and increase fall risk. Diuretics, beta blockers, anticonvulsants, anti-hypertensives, benzodiazepines, and antidepressants should be avoided in individuals with a significant fall risk or a history of fall. (See Beers Criteria, page 51).
With the exception of gabapentin and pregabalin, podiatrists seldom prescribe these high-risk medications; however, Eckles said that podiatrists need to assess medications in all patients that have fallen or are at risk for falls. Close monitoring is recommended to determine whether the therapeutic benefit outweighs adverse events.
| Psychosocial factors |
Fear of falling is often overlooked as a fall risk in older adults. “Every adult over the age of 70 has had a friend or family member who has been injured by a fall,” said Eckles. “As a result, these individuals stiffen when they encounter wet or uneven surfaces, or obstacles.” By adopting this stiffening strategy, a person with heightened fall anxiety reduces range of motion and with it, his/her ability to adapt to environmental challenges.
Like people who are afraid of falling, “people who are depressed fall more than those who are not depressed,” explains Eckles. In general, these individuals live alone, have multiple health issues, are home-bound or are isolated.
“…one survey of older adults… found that 26% of men and 47% of women had not had footwear size measured in more than 5 years.”
| Falls Risk Assessment |
Gait and balance disorders are a major cause of falls and a consistent predictor of future falls. Early screening for gait and balance disorders and initiating appropriate intervention are important steps because interventions may prevent further disability and loss of independence. If an older adult reports a fall, the Centers for Disease Control and Prevention recommends that they be evaluated for evidence of:
- Gait and balance dysfunction
- Lower extremity weakness
- Dizziness
- Adverse drug events
- Foot/shoe problems
- Poor visual acuity
- Household safety hazards
Time is a major barrier to effective fall risk evaluation for many physicians. Many physicians forgo screening because they think risk assessments take too much time. In addition, many are unaware that falls prevention services are reimbursable and do not require a specific code. “No one performs the Timed Up and Go (TUG) test because they think it is too time consuming,” explained Eckles.
On the contrary, TUG is a highly validated assessment that can be administered in about 10 seconds and is a reliable diagnostic tool for gait and balance disorders. It measures the time that it takes for a person to rise from a chair, walk three meters, return to the chair, and sit back down. A score of ≥ 14 seconds indicates a high risk of falls.
| Interventions to Reduce Falls |
Due to the multifactorial nature of gait and balance disorders, several types of treatments are usually needed to restore, maintain, or improve physical health. “Every adult 65 and older should be regularly assessed for fall risk to identify the types of interventions required, even if they have not yet experienced a fall,” said Thurmon Lockhart, PhD, Professor of Biomedical Engineering at Arizona State University.
Targeted interventions can reduce falls by 30% to 40%. Eckles suggested that, at minimum, these interventions focus on pain management, improving footwear, exercise habits, depression screening, bone screening, and a review of current medications.
Patients with gait and balance issues are referred to a physical therapist for further evaluation of the patient’s mobility status and functional level. Physical therapy is effective for targeting gait, posture, or strength deficits. “Improvements can be seen in as little as 4 to 6 weeks, depending on the intensity of therapy,” said Johnson. However, gains are much more difficult to attain in older adults who are sedentary, have dementia, or are not adherent to therapy, she explained.
“Shoes and flooring are major barriers to compliance,” said Eckles. Therefore, it is important to get caregivers involved in making the living environment safe.
Nearly 80% of older adults have foot pathologies, including bunions, calluses, and hammertoes that are caused by shoes that unevenly distribute plantar pressure. Low-heeled, slip-resistant shoes with a wider and higher toe box improve balance by stabilizing the foot and reducing plantar pressure.
Access to appropriate footwear may be a challenge for many older adults because of their fixed income or because customized shoes are not readily available in most retail stores. Orthotics are a low-cost, widely available intervention for improving balance and preventing falls in older adults. A recent study of adults ≥ 65 years of age demonstrated sustained balance improvements—as measured by the Berg Balance Scale and TUG test—after 4 weeks of using flat or textured insoles, as compared to the control group without insoles.
| Paradigm shift: Focus on prevention |
Technology—virtual reality, smart homes, and apps—is being used to motivate individuals and prevent falls before they happen.
There is a lot of excitement surrounding smart-home technology which uses sensors on walls and floors to collect data about the person’s gait, posture, number of falls, and instability. These sensors can be used to monitor and assess daily activities in older adults who are at high risk for falls. Lockhart explained that there is some evidence that using this technology may help prevent falls in older adults.
Preservation training is another area of growing research in falls prevention. Early research from Lockhart’s group at Arizona State University demonstrated that humans possess an innate adaptive behavior which reduces the likelihood of slips, trips, and falls after the first incident. He calls this behavior kinetic learning.
Findings from these studies led his team to develop a slip simulator which is marketed by Industrial Biodynamics and used by top companies such as UPS and General Electric to reduce workplace falls.
The Slip SimulatorTM is currently being used to train UPS drivers to safely walk in inclement weather conditions. Employees who received this training reduced their risk of falls by 70%.
Armed with these findings, Lockhart’s team is now applying the Slip SimulatorTM technology to older adults with Parkinson’s disease. In an article currently under peer review for publication, the group reports positive changes in posture and stability in patients with Parkinson’s disease.
| The Future of Falls Prevention |
“There is no doubt that early screening and appropriate interventions can mitigate fall risk,” said Lockhart. “However, we need to get to the point where we can prevent falls all together.”
Source Lower Extremity Review
| References |
- Home and Recreational Safety: Important Facts about Falls, Centers for Disease Control and Prevention (CDC). Updated February 10, 2017. Accessed January 30, 2019
- Algorithm for Fall Risk Screening, Assessment, and Intervention, PDF, Centers for Disease Control and Prevention (CDC). Updated March 24, 2017. Accessed January 30, 2019.
- Gait and balance disorders in older adults, Salzman B. Am Fam Physician. 2010 Jul 1;82(1):61-8. Full text
- Biomechanical walking pattern changes in the fit and healthy elderly, Winter DA, Patla AE, Frank JS, Walt SE.
Phys Ther. 1990 Jun;70(6):340-7. PDF - Stride-dependent changes in gait of older people, Elble RJ, Thomas SS, Higgins C, Colliver J. J Neurol. 1991 Feb;238(1):1-5.
- Fall Risk and Podiatric Intervention, PDF, Eckles R. Podiatry Management. 2016; April-May:161-169.
- Incorrectly fitted footwear, foot pain and foot disorders: a systematic search and narrative review of the literature, Buldt AK, Menz HB. J Foot Ankle Res. 2018 Jul 28;11:43. doi: 10.1186/s13047-018-0284-z. eCollection 2018. Review. Full text
- A Pocket Guide to the AGS 2015 Beers Criteria, PDF, The American Geriatrics Society (AGS). Pocket Published 2015. Accessed January 30, 2019.
- Interventions for the prevention of falls in older adults: systematic review and meta-analysis of randomised clinical trials, Chang JT, Morton SC, Rubenstein LZ, Mojica WA, Maglione M, Suttorp MJ, Roth EA, Shekelle PG. BMJ. 2004 Mar 20;328(7441):680. Review. Full text
- A sustainable programme to prevent falls and near falls in community dwelling older people: results of a randomised trial, Steinberg M, Cartwright C, Peel N, Williams G. J Epidemiol Community Health. 2000 Mar;54(3):227-32. Full text
- Evaluating Problems With Footwear in the Geriatric Population, Ikpeze TC, Omar A, Elfar JH. Geriatr Orthop Surg Rehabil. 2015 Dec;6(4):338-40. doi: 10.1177/2151458515608672. Full text
- The effect of flat and textured insoles on the balance of primary care elderly people: a randomized controlled clinical trial, de Morais Barbosa C, Bértolo MB, Gaino JZ, Davitt M, Sachetto Z, de Paiva Magalhães E. Clin Interv Aging. 2018 Feb 19;13:277-284. doi: 10.2147/CIA.S149038. eCollection 2018. Full text
- Smart homes and home health monitoring technologies for older adults: A systematic review, Liu L, Stroulia E, Nikolaidis I, Miguel-Cruz A, Rios Rincon A. Int J Med Inform. 2016 Jul;91:44-59. doi: 10.1016/j.ijmedinf.2016.04.007. Epub 2016 Apr 19. Review.
- Reduce Slips, Trips, and Falls By Up to 70%, Industrial Biodynamics, Slip Simulator.TM Accessed January 30, 2019.
- The mental representation of the human gait in young and older adults, Stöckel T, Jacksteit R, Behrens M, Skripitz R, Bader R, Mau-Moeller A. Front Psychol. 2015 Jul 14;6:943. doi: 10.3389/fpsyg.2015.00943. eCollection 2015. Full text
- Gait Analysis: Normal and Pathological Function, Monitoring Editor: Jacquelin Perry and Judith M. Burnfield. ISBN: 978-1556427664, 2010, Slack Incorporated, New Jersey. $92.95, 551 pages, hardcover