Wanted: Accessible homes for Ontarians of all ages and abilities
Nearly 2 million Ontarians live with some form of disability that affects their mobility, vision, or hearing — and the country is aging at a faster rate than ever before. That’s why experts are saying we need to embrace universal design.

St. Catharines resident Diane Foster, 67, has been using a wheelchair for 12 years. Kevin Spurgaitis TVO
By Kevin Spurgaitis, TVO December 16, 2019
ST. CATHARINES — Diane Foster doesn’t have it easy coming and going from her modest brick-and-siding bungalow in St. Catharines. The four stairs leading up to the front entrance can’t accommodate her wheelchair; over the years, the lift to the back door has rusted out, seized up, or broken down altogether. And the home’s interior presents its own challenges.
“My house was built in 1919, and, over the years, I’ve required many modifications to my home,” says Foster, 67, who lives alone and has fibromyalgia, osteoporosis, three forms of arthritis, and spinal stenosis — a condition that results in the narrowing of the spinal canal — and has been using a wheelchair for 12 years. “Originally, I had a clawfoot bathtub in here, which, of course, I couldn’t get in and out of… I also removed my bedroom door and lowered the light switches.” But Foster’s house, which is filled with the usual household furnishings and keepsakes — family photos, plush toys — “simply isn’t big enough to accommodate” her power wheelchair, which is easier to manoeuvre than her standard one.”
It would be better, she says, if her 750-square-foot house were open-plan — or if it at least had wider passageways and doorways, low thresholds, and rooms large enough for either of her wheelchairs. What’s more, smooth floors, easy-to-operate windows, storage and work surfaces that are easy to see and reach, and stainless-steel handrails (which, she says would mean that she wouldn’t need to “wall and furniture surf” whenever she needs to get up from her wheelchair) would improve her quality of life significantly.
“What about those of us who have owned their own home for a number of years and don’t want to move just because we have a disability?” she asks. “I’d like to be able to afford to improve this house to make it more accessible.”
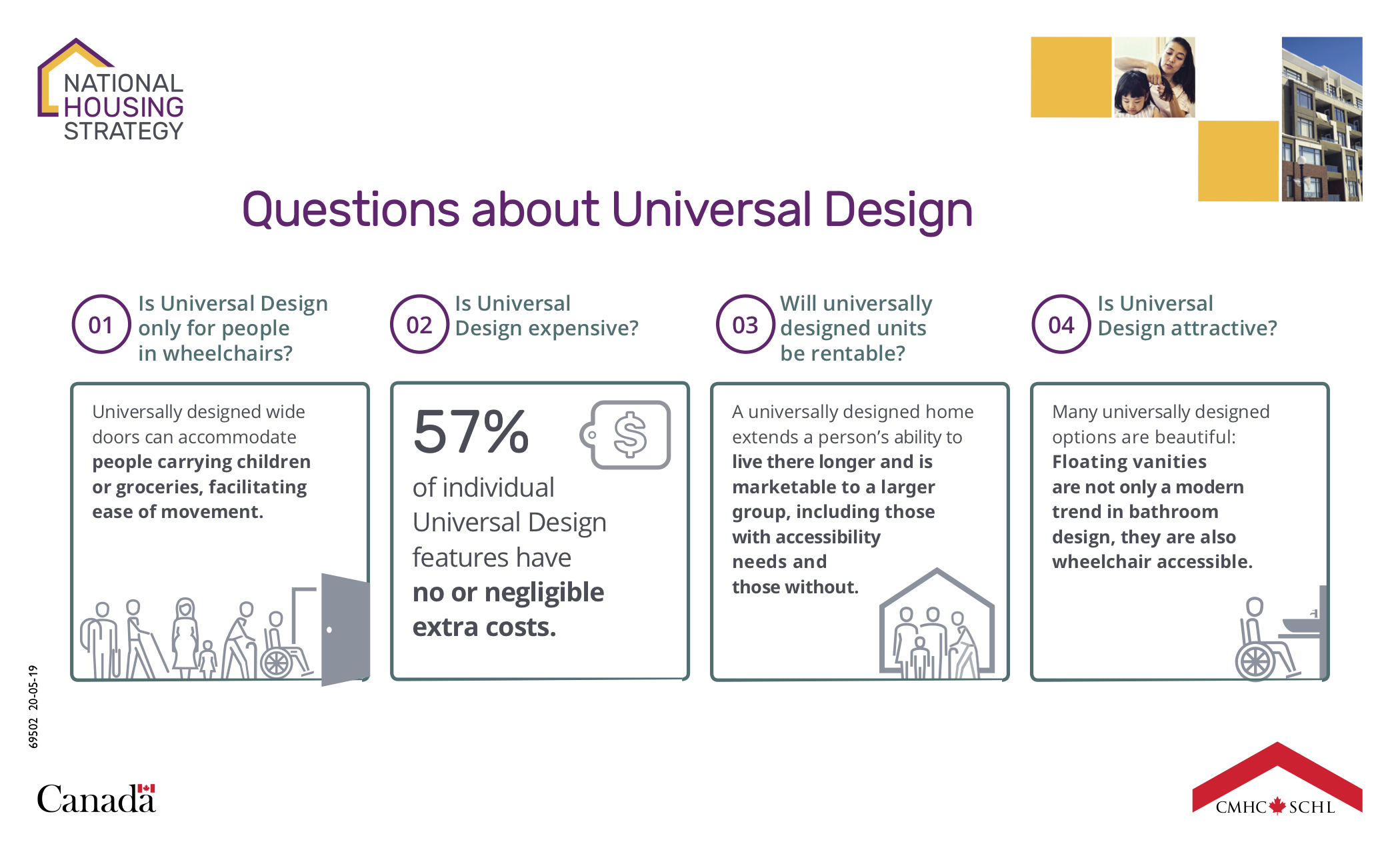
The kinds of features Foster is talking about form part of an approach known as universal design. The demand for universally designed homes has grown in recent years in Ontario and the rest of Canada, and, partly thanks to the aging baby-boomer demographic, it’s expected only to increase. Although recent federal and provincial legislation has included more provisions for people with disabilities, and updated building codes have provided basic safety standards, disability advocates say that they don’t take into account all the needs that arise from the differences in human characteristics and abilities — and they’re calling for the wider application of universal-design principles.
Architect and educator Ron Mace, who coined the term in the 1980s, has said that the approach involves “designing all products and the built environment to be aesthetic and usable to the greatest extent possible by everyone, regardless of their age, ability, or status in life” — allowing more residents to engage easily and intuitively with their environments, even as their abilities and needs change over time. This means doorways at least 36 inches wide and hallways at least 42 inches wide, non-slip flooring, easy-access storage, raised front-loading appliances, low- or no-threshold stall showers, and at least one step-free entrance. Other accessible design features include lever-style door handles and faucets, and easy-to-use rocker light switches.
“ is friendly, useable, and caters to just about everybody from the time that they’re an adolescent up to the time that they’re a senior, especially someone living with Alzheimer’s,” says Sandy Faugh, the team lead for AccessAbility Advantage, a proprietary service that consults on accessibility strategy as part of March of Dimes Canada. “That’s not only good for people with disabilities, especially seniors,” she says. “It’s good for the parent that’s pushing their child in a stroller and the person who has just undergone a hip replacement or busted their collarbone — both of whom find out pretty darn fast how non-accessible their home is.”
The Canada Mortgage and Housing Corporation, the country’s housing agency, has had an eye on accessibility for a number of years. As part of the CMHC National Housing Strategy, organizations can access certain funds if they can show that their projects involve a certain level of accessibility that’s going to help people with disabilities. “Universal design is getting more attention now, as there’s more of a need for it and a lot more examples of it,” says Arlene Etchen, a regional consultant at the CMHC who focuses on accessibility and outreach. “And we know that’s only expected to increase.”
Nearly 2 million Ontarians — or about 15 per cent of the population — live with some form of disability that affects their mobility, vision, or hearing, according to Statistics Canada. Across the country, the number of people with a physical disability is expected to increase from roughly 3 million — or 10 per cent of the population — to nearly 4 million by 2030. And, with one in six Canadians now over the age of 65, the country is aging at a faster rate than ever before, StatsCan says.

Diane Foster with her service dog, a black Labrador retriever named Olla. Kevin Spurgaitis TVO
On Foster’s bathroom wall hangs a small red and white canvas that reads “Life is a beautiful ride.” She says that she was a healthy, active grandmother who cycled about 5,000 kilometres every summer, walked everywhere all winter, and played several musical instruments. Then, one “devastating morning” in 2009, she couldn’t get out of bed.
Foster says that she didn’t know which was worse when it came to her psoriatic arthritis: the pain from staying in one position or the pain of trying to move at all. She could no longer turn a door handle, hold a pen, lift a book, comb her hair, or brush her teeth. In a way, it felt as if her own body had “betrayed” her, she says.
“I tried to retain my independence but soon realized that I was unable to do the simple tasks required for daily living,” Foster says. “My life changed drastically. I went from being self-sufficient to being totally dependent on others.”
Medication now makes the pain tolerable, Foster says — and she receives help from three personal support workers who visit her twice daily in rotation.
“If my kitchen was more accessible, at least, I’d be able to prepare my own meals and not wait for somebody to prepare them for me,” says Foster, who is co-chair of St. Catharines Accessibility Advisory Committee.
Through the CMHC and March of Dimes Canada Assistive Devices Program, she’s been able to make modifications to her century home that have cost tens of thousands of dollars. But, as her monthly Old Age Security pension payment is about $1,400, she can’t afford to remove the other barriers — and doing so could cost tens of thousands of dollars more. Even if she wanted an affordable, accessible apartment, most would not be large enough for her service dog, a black Labrador retriever named Olla, and mobility equipment. And the wait times for such units are between 10 and 15 years.
“I’d never burden my with having to look after me, and I’m not old enough to go into a seniors’ residence,” she says. “I’m comfortable in my own home. I’d just like to be able to access it.”
| What is the Assistive Devices Program? March Of Dimes Canada. Posted on Youtube Nov 22, 2019 |
Rebekah Churchyard, acting president of the Toronto Council on Aging, which, as part of the Councils on Aging Network of Ontario, works to address issues facing older adults, says that “it’s an excellent symbol both for our global and national health that we’ve now got unprecedented longevity.” But, she adds, “we’re living in a world where, increasingly and painfully, it’s obvious that people need to remain in particular spaces — or visit others — and they simply can’t anymore.”
Churchyard points to the concept of “aging in place,” which is about the maintenance of an older adult’s independence and choice to live in their home. “Maybe it’s their matrimonial home, maybe it’s their own home, or maybe it’s their home shared with friends,” she says. “But every single older person who I have ever spoken with has a very strong desire to stay in their home — and ‘age in place’ there — as long as possible. We have to start planning for it now.” And, she notes, “What we’re not always considerate of is the cost of their built environment within the home… There isn’t a whole lot of base funding for the increasingly aging population.”
But she says that she’s “enthused and encouraged” by how public systems have supported people with physical differences and intellectual differences in recent years: “In that respect, governments have done a better job than ever before to promote accessible environments.”
Ontario made Canadian history when it passed the Accessibility for Ontarians With Disabilities Act in 2005. The AODA mandates that the province develop accessibility standards in areas such as built environments and ensure that the public and private sectors meet them by 2025. Still, despite the province’s 2015 accessibility action plan — called “Path to 2025” — the implementation of the AODA has fallen behind in recent years, according to such consumer-advocacy groups as the AODA Alliance.
In 2015, changes to the Ontario Building Code also came into effect, essentially upping accessibility requirements for multi-unit residential buildings. Fifteen per cent of all new units — and the majority of renovations — must incorporate basic accessibility features, such as barrier-free entrances. Living rooms, kitchens, bedrooms, and bathrooms must be large enough to allow a wheelchair to turn around within them, and feature reinforced walls to accommodate grab bars and other assistive devices. Visual fire alarms are now mandatory, too.
But the province’s building code doesn’t apply to existing houses or to new single-family or semi-detached homes or townhomes. And the rules don’t produce benefits for everyone: kitchen counters remain unreachable for some, while acoustics present challenges for others.
According to Faugh, it costs only 2 per cent more to build an accessible home. “It doesn’t cost you anything to make a four-foot hallway instead of a three-foot hallway,” she says. “You’re just placing the walls in a different spot, right?”
Some municipalities, such as Caledon, have gone ahead and adopted universal-design policies. Developers looking to build there must offer a model or drawings based on universal design, according to the CMHC. And, in 2015, Deep River created the Citizen Housing Advisory Committee to help come up with new policies and procedures that would accurately represent older people’s “needs, wants, and values.”
These are “small steps” in the right direction, Etchen says. And, according to the UK-based social-housing provider Habinteg, such steps can pay dividends: its research shows that universal design reduces social isolation, prevents extended hospitalization and long-term unemployment, and facilitates the economic participation of people with disabilities.
Building accessible homes while retrofitting others is about getting the “right players at the table” so that they can actually “drive a doable solution for the residential market,” Faugh says. “We’ve got to show the architects, the engineers, the designers, and the interior designers what universal and accessible design looks like, teach them to do things a little bit differently and make that the new standard right off the bat.”
In the meantime, both March of Dimes Canada and the CMHC recommend that seniors and people with disabilities — and their friends, families, and neighbours — consider various low- to no-cost modifications, including painting thresholds in a contrasting colour to create a visual signal for anyone with impaired vision, removing the storm or screen doors to make entry easier for those with arthritis or limited upper-body strength, using swing-away hinges to allow an extra few inches of clearance for a wheelchair or walker, and merely removing any obstacles, such as area rugs, from hallways and main rooms.
A smile flashes across Foster’s face as she approaches her wheelchair lift after a short outing. She admits that it doesn’t take very long to lower and raise it during the warmer seasons. But it can “feel like an eternity” in the ever-deepening cold.
“Maintaining my independence is part of maintaining my dignity and just being respected as a functioning, contributing member of society,” Foster says.
For her, the question remains whether more governments, businesses, and organizations will get behind people with disabilities — who are already taking active roles in their own communities — and commit to accessibility plans that’ll make universally designed homes more widespread in the years to come. After all, Foster says, universal design “does help everybody.”
| Kevin Spurgaitis is a Toronto-based freelance writer and editor. His work has appeared in the Globe and Mail, the Toronto Star, and the Guardian, among others. Follow @KevinSpurgaitis |
Source TVO
| Further reading |
Home Environment, Living Alone, and Trajectories of Cognitive Function Among Older Adults With Functional Limitations, Park S, Kim B, Amano T, Chen Q. Environment and Behavior. 2019. https://doi.org/10.1177/0013916519879772
Person-Environment Fit Approach to Trajectories of Cognitive Function Among Older Adults Who Live Alone: Intersection of Life-Course SES Disadvantage and Senior Housing, Park S, Kwon E, Kim B, Han Y. J Gerontol B Psychol Sci Soc Sci. 2019 Aug 21;74(6):e1-e12. doi: 10.1093/geronb/gbz025.
Aging in Place of Vulnerable Older Adults: Person-Environment Fit Perspective, Park S, Han Y, Kim B, Dunkle RE. J Appl Gerontol. 2017 Nov;36(11):1327-1350. doi: 10.1177/0733464815617286. Epub 2015 Nov 26.
Age-friendly environments and life satisfaction among South Korean elders: person-environment fit perspective, Park S, Lee S. Aging Ment Health. 2017 Jul;21(7):693-702. doi: 10.1080/13607863.2016.1154011. Epub 2016 Mar 3.
The effects of health on the life satisfaction of poor and nonpoor older women in Korea, Park M, Kim J, Park B. Health Care Women Int. 2014;35(11-12):1287-302. doi: 10.1080/07399332.2014.888064. Epub 2014 Mar 20.
Examining the relationship between communities’ ‘age-friendliness’ and life satisfaction and self-perceived health in rural Manitoba, Canada, Menec VH, Nowicki S. Rural Remote Health. 2014;14:2594. Epub 2014 Jan 18. Full text
Also see
Modifications to social, physical spaces make living at home easier for older adults Washington University in St. Louis