Development of the arch: functional implications
Contrary to the conclusions of early research, recent studies suggest that arch height does indeed affect lower extremity function. The biomechanics associated with different arch heights may provide a basis for treatment and prevention of related injuries.

By Thomas C. Michaud, DC, Lower Extremity Review July 2012
The easiest way to categorize foot structure dates back to Galen, when feet were classified simply by the height of the medial longitudinal arch. The long-held belief is that arch height significantly influences foot function: low-arched feet are considered hypermobile and susceptible to pronation-related injuries while high-arched feet are usually described as stiff and prone to high-impact injuries.
Although injury patterns support the theoretical link between arch height and function (e.g., low-arched individuals frequently present with medial knee and ankle injuries, while high-arched individuals are more likely to suffer stress fractures), early research by Nigg et al,[1] questioned the connection between arch height and 3D motion.
Using calipers to evaluate the height of the medial longitudinal arch, these researchers performed 3D imaging on 30 volunteers and found no correlation between arch height and foot function: individuals with high arches frequently presented with increased calcaneal eversion while low-arched individuals often possessed rigid, less mobile feet.
Unfortunately, although their 3D analysis was extremely detailed, Nigg et al’s use of calipers to measure arch height was regrettable because caliper measurements are easily distorted by hypertrophy of the arch muscles and/or obesity, which significantly alter arch shape. Because the authors may not have identified true arch height, the findings of this study provided little insight into the connection between arch height and motion.
| Figure 1: Posterior view of left calcaneus. In a well-developed arch, the sustentaculum tali (ST) forms with an upward angulation (A) that positions the talus directly above the calcaneus. When excessive pronation occurs during childhood, the sustentaculum tali often forms with a downward slope (B), which limits its ability to support the talus. |
In 2001, Williams and McClay [2] finally resolved the controversy regarding arch height and 3D motion. Using a highly reliable method of quantifying arch height (arch height ratio) these researchers performed 3D motion analysis on high- and low-arched runners. They demonstrated conclusively that arch height and function are indeed correlated: people with low arches have greater rearfoot eversion excursions and velocities than people with high arches, who present with increased vertical loading rates.
In a follow-up study,[3] these authors determined that arch height was also predictive of injury: low-arched runners exhibited more knee, soft tissue, and medial injuries (e.g., adductor strain, medial knee and ankle injury, and sesamoid/first metatarsophalangeal joint injury), while high-arched runners had a greater prevalence of bony injuries (e.g., stress fractures) and lateral injuries (e.g., greater trochanter bursitis, iliotibial band friction syndrome, and/or lateral ankle sprains).
According to Gould et al,[4] formation of a healthy medial longitudinal arch requires the formation of a well-developed sustentaculum tali, a healthy tibialis posterior tendon, an adequate deltoid ligament, a non-constricted Achilles tendon, and a properly placed inferior calcaneonavicular ligament. These authors note that development of the arch is not complete until the age of 8 years and that hyperpronation, often secondary to genu valgum, is the norm for 5-year-old children.
| Barefoot benefits |
Though rarely discussed, barefoot activity has been shown to facilitate arch development. In a study of 2300 children aged 4 to 13 years and raised in rural India, Rao and Joseph [5] used static footprints to evaluate the influence of footwear on medial arch development. They discovered that children raised without shoes rarely presented with low arches: by age 13, only 2.8% of the barefoot children had flat feet compared with an 8.6% prevalence of flat feet in the children wearing shoes. (The two groups of children were similar with regard to body weight and other factors that contribute to flat feet). The prevalence of low arches also varied with the type of shoe worn: children wearing closed-toe shoes had lower arches than the children who wore sandals.
The authors suggested that because children wearing sandals were more likely to kick them off to play than those wearing closed-toe shoes, the resulting interludes of unshod activity may have accounted for the lower prevalence of low arches in this group. The study was interesting as it revealed a clear tendency for arch height to increase with age; e.g., 14.9% of children aged 6 years had low arches while only 5.3% of 9-year-olds, 3.3% of 11-year-olds, and 2.2% of 12-year-olds presented with low arches. Because of the higher prevalence of low arches among children aged 6 years who wore shoes compared with those who did not, the authors concluded that the critical period for arch development is before age 6.
I believe this important research confirms that sensory stimulation associated with barefoot activity may produce a protective increase in muscle tone that is capable of elevating the arch. This is consistent with research by Robbins and Hanna,[6] who found that barefoot activity produced measurable increases in adult arch height as seen on weight-bearing x-rays. The protective increase in tone is invaluable in children, as it may permanently alter bony architecture by allowing for development of a healthy sustentaculum tali. Because obesity increases the potential for flatfoot, closely monitoring development of the medial longitudinal arch in overweight children is imperative, particularly for children aged 4 to 7 years.
As demonstrated by Gould et al,[4] excessive pronation before age 7 (when the sustentaculum tali is fully ossified) may mold the sustentaculum tali so that it forms with a downward slope, making it incapable of supporting the talus adequately (Figure 1). Development of the sustentaculum tali is essential for the formation of a functional medial longitudinal arch because it allows the bony architecture to control motion, thereby lessening muscular/ligamentous strain during stance. Because the typical developmental genu valgum present in children aged 2 to 3 years straightens between 4 and 6 years (reducing the medial displacement of body weight responsible for maintaining a low arch), barefoot activity at this time may increase muscle tone, allowing for the formation of a healthy arch.
In situations in which barefoot activity is not possible or when the child is significantly overweight, incorporating prefabricated or custom foot orthoses may be indicated as they may enhance development of the medial arch by lifting the talus off the sustentaculum tali, allowing for normal development of this important bony projection.[8]
| Causes of flatfoot |
Although not discussed in detail here, as they are uncommon and often treated with surgical intervention, certain pathological deformities such as the vertical talus, skew foot, or tarsal coalition may result in extreme flatfoot deformities. The well-trained practitioner should be able to differentiate these conditions from the nonpathological flatfoot and make the appropriate orthopedic referral.
| Figure 2. (A): The poorly developed sustentaculum tali is unable to adequately support the talar head. Adapted from tracings of x-rays as illustrated in Hypermobile flatfoot with short tendo Achilles, Harris RI, Beath T. J Bone Joint Surg Am 1948;30(1):116-138. (B): Ideal development of the sustentaculum tali. |
While pathological flatfoot deformities are rarely seen in-office because they are typically treated during the first few months of life, Harris and Beath [9] describe a type of low arch known as a hypermobile flatfoot that is frequently seen in clinical settings because the condition is often symptomatic. In addition to a low arch, this deformity can be identified by the increased range of forefoot inversion (the midtarsal joint may allow as much as 50° of forefoot inversion), and rearfoot eversion (the calcaneus is often everted more than 10° during static stance). Most notably, ankle dorsiflexion is dramatically reduced; negative 25° of ankle dorsiflexion as measured with the talonavicular joint maintained in a neutral position is not uncommon.
According to Harris and Beath [9] the hypermobile flatfoot results from an inherited malformation in which the sustentaculum tali forms a tongue-like process that projects proximally (Figure 2). The authors note that a superior/inferior x-ray is a useful index for determining the degree of the deformity, as it demonstrates a shadow where the head of the talus is not supported by the anterior calcaneus (e.g., compare the shaded area in Figure 2A to the shaded area in Figure 2B. The malformed sustentaculum tali is unable to support the head of the talus, and superimposed body weight allows the talus to adduct and plantar flex while the calcaneus simultaneously everts. The excessive talar plantar flexion only serves to amplify the instability as the head of the talus behaves like a wedge that further separates the incompetent sustentaculum tali from the navicular bone.
Because the plantar ligaments are often unable to contain the head of the talus, the medial arch may collapse completely, allowing the talar head to make ground contact. This produces a paradoxical decrease in symptoms as the ground now supports the talus, lessening strain on the plantar talonavicular ligaments (the ground essentially acts as an orthotic device). According to Harris and Beath,[9] individuals with this deformity often learn to avoid sports and strenuous activities. Although symptoms such as painful joints and fatigued muscles may be delayed indefinitely with a sedentary lifestyle, foot pain and discomfort most often begin by the early teenage years and may be evident in children as young as 5 years.
Whereas the hypermobile flatfoot represents a relatively uncommon genetic cause for the formation of a flattened medial longitudinal arch, reduced arch height may also result from less serious conditions, such as an unstable first ray, a malformed midtarsal joint, or a tight Achilles tendon. Regardless of the precise cause, once a low arch is formed it can significantly alter motion through the entire kinetic chain.
| Biomechanical effects |
In their 3D study of runners presenting with high and low arches, Williams et al,[10] confirm that, compared with people with high arches, individuals with low arches are more likely to make initial ground contact with a greater degree of rearfoot inversion. A lateral heel contact may represent a learned protective mechanism because excessive inversion of the calcaneus at touchdown provides the tibialis posterior muscle more time to dampen subtalar pronation by allowing the rearfoot to move through a larger range of motion. This may explain why runners who strike on the lateral side of the heel are less likely to incur injuries11 and why lifelong runners who have never been injured are more likely to strike the ground with the rearfoot inverted excessively than runners who strike with a vertical or everted rearfoot.[12]
After striking the ground, the calcaneus in low-arched individuals everts 32% faster than in people with high arches.10 The increased eversion velocity may be troublesome as it places greater strain on the restraining muscles and ligaments. In fact, some authors suggest the angular velocity of subtalar joint pronation may play a more important role in various injuries than the overall range of pronation.[13]
The combination of a low arch and a tibial varum is troublesome because excessive rearfoot inversion at heel strike forces the subtalar joint to pronate rapidly through a very large range of motion. Because subtalar pronation reaches peak angular displacement during the first half of the contact period, it is common for the subtalar joint to move through a 16° range of motion in the first 0.08 seconds of the contact period.[14,15] For the individual to remain injury free, the rapid, sometimes extreme range of motion associated with subtalar joint pronation must be dampened by the supporting muscles and ligaments. A series of potential injuries associated with excessive contact period pronation is illustrated in Figure 3.
| Figure 3: Potential injuries associated with excessive subtalar pronation. As the subtalar joint pronates, the talus is forced to adduct and plantar flex excessively (A) while the calcaneus simultaneously everts. These actions markedly strain the calcaneonavicular ligament (the sling ligament) and the plantar talonavicular joint capsule. Over time, these exaggerated movements can lead to a pathologic laxity of these tissues. In addition, excessive subtalar pronation may damage the medial band of the plantar fascia as the talus is displaced anteriorly approximately 1.5 mm with every 10° of calcaneal eversion (B). Manter [31] likens this to the forward motion of a right-handed screw placed directly along the subtalar joint axis: as the calcaneus everts, the screw tightens, pushing the talus anteriorly. This forward motion is insignificant in an average foot but may play a critical role in the pathomechanics associated with excessive subtalar joint pronation, as the anterior displacement of the talus causes the navicular bone and first three rays to move forward and abduct relative to the fourth and fifth rays (C). The forward motion of the medial column irritates the medial plantar fascia since it places a tensile load on this relatively inelastic tissue that may exceed its functional ability to elongate. The flexor digitorum brevis may be strained as it attempts to resist forward motion of the medial column by eccentrically contracting. This could increase tractioning of the flexor digitorum brevis muscle’s periosteal attachment, eventually resulting in a heel spur. The abductory movement of the medial column may also be responsible for injury because it creates a compressive force at the junction of the medial and lateral column. This may lead to chronic inter-metatarsophalangeal bursitis at the third interspace (D). |
In addition to producing various injuries in the medial foot, excessive subtalar pronation may also be responsible for producing injury up the proximal kinetic chain. The tibialis posterior tendon is particularly prone to injury because of its long lever for controlling subtalar motion, and is therefore exposed to greater tensile strains than muscles working through shorter lever arms. This explains why clinically we so often see individuals with hypermobile flatfeet present with tibialis posterior tenosynovitis. It is also consistent with prior research showing that excessive subtalar pronation is causally related to medial tibial stress syndrome.[13,16]
| Figure 4: Superior view of right lower extremity: Excessive internal rotation of the femur (A) drives the lateral femoral condyle into the lateral patellar facet (B). |
Despite the fact that low arches convert a smaller percentage of frontal plane rearfoot motion into tibial rotation than high arches, the transferred rotation is still capable of injuring the tibia, perhaps because of the increased velocity of calcaneal eversion.10 In a study of 320 cases of stress fractures in athletes, Matheson et al,[17] noted a clinical connection between excessive pronation and lower tibial stress fractures. More recently, Milner et al,[18] performed 3D analysis on runners with and without a prior history of tibial stress fracture and determined the stress fracture group moved through stance phase with greater degrees of rearfoot eversion. It is possible that, because the lower tibia has a lower polar moment of inertia,19 it is less able than the rest of the tibia to resist torsional strains associated with excessive pronation and is therefore more prone to developing stress fractures.
| Figure 5: The combination of a low arch (A) and an anteverted hip often results in excessive internal rotation of the entire lower extremity (B), which greatly increases valgus collapse at the knee (C). These actions increase tensile strain on the anterior cruciate ligament (ACL), the medial collateral ligament (MCL), and the posterior oblique ligament (POL). The semimembranosus muscle (SM) plays an important role in stabilizing the medial knee. The combination of excessive foot pronation, valgus knee alignment, and femoral anteversion are collectively referred to as “the miserable malalignment syndrome,” since they significantly increase the potential for valgus collapse at the knee. |
| Effects at the knee |
While the effects of excessive pronation on the foot and ankle are relatively straightforward, the effect of contact period pronation on knee motion is less obvious. Even though people with low arches move through larger ranges of calcaneal eversion than people with high arches because they convert a smaller percentage of rearfoot eversion into tibial rotation, the overall range of tibial rotation present during stance phase is about the same in people with high and low arches.[10] Clinical research confirms that people with low arches are more likely to develop retropatellar pain [20] and knee osteoarthritis,[21] but the exact mechanisms remain unclear.
In an attempt to understand the connection between subtalar pronation and knee pain, LaFortune et al,[22] surgically inserted intracortical rods into the proximal tibia, distal femur, and central patella of five volunteers. Target clusters attached to these rods allowed researchers to measure the exact degree of rotation present between the bones of the lower extremity as participants walked on a treadmill wearing insoles fitted with varus posts (to decrease pronation) and valgus posts (to increase pronation).
When wearing the valgus-posted midsole, tibial internal rotation increased 4° more than with the varus midsole. The surprising aspect of this study was that the valgus posts, which increased the range of subtalar pronation, produced no appreciable change in the degree of tibiofemoral joint rotation. This means that as the valgus post forced the tibia to internally rotate, the femur completed the exact same degree of rotation so that no net rotation occurred at the tibiofemoral articulation: all of the transverse plane motion induced at the foot by the valgus post traveled through the knee and was absorbed by the hip. The clinical implication of this research is that excessive pronation is more likely to stress the hip and pelvis than the tibiofemoral joint.
The most important finding of the research by LaFortune et al,[22] is that it may explain the connection between excessive pronation and lateral retropatellar pain. The researchers noted the internally rotating femur displaced the lateral femoral condyle into the lateral patellar facet (Figure 4). LaFortune et al,[22] also made the surprising observation that, as the foot was forced to pronate by the valgus wedge, the tibia shifted an additional 2 mm medially relative to the femur in the frontal plane. This is significant since the medial shift of the tibia relative to the femur increases tensile strain on the anterior cruciate ligament (ACL), which could partly explain the clinical connection between excessive foot pronation and an increased prevalence of ACL injuries.[23]
While the individuals in the LaFortune’s study had increased ranges of calcaneal eversion with valgus posts, the researchers’ findings do not explain the clinical connection between low arches and knee pain, as the typical low-arched person does not present with excessive tibial rotation. Perhaps it is the increased speed of pronation associated with low arches that increases injury risk. It is also possible that low arches affect only the proximal structures when they occur in combination with other factors that increase lower extremity malalignment; e.g., weakness of the hip external rotators, genu valgum, and/or anteverted hips.
The combination of low arches and anteverted hips is particularly troublesome as it is almost always associated with excessive valgus collapse at the knee, which may be extreme, particularly when running and jumping. This greatly increases the likelihood of injuring the ACL, the medial collateral ligament, and/or the posterior oblique ligament because valgus collapse at the knee increases tensile strain on these important structures (Figure 5).[24]
To be comprehensive, conservative treatment should include custom or prefabricated orthoses to decrease the effect of foot pronation on the distal aspect of the kinetic chain, along with specific exercises to control motion at the hip. Because varus wedges are often less effective at reducing valgus collapse when used on people with low arches,[25] it is essential that individuals with anteverted hips and flat feet be treated with specific strengthening exercises and agility drills. In a study evaluating the efficacy of these drills in 1435 Division I college female soccer players, Gilchrist et al,[26] determined that athletes incorporating a series of simple on-field alternative warm-ups prior to participating in sport had a 70% reduction in the rate of noncontact ACL injuries. The specific drills used in that study are outlined in Table 1. Similar injury prevention programs have been described by others.[27,28] Because of their proven efficacy, this type of regimen should be recommended for all individuals presenting with even a slight tendency for valgus collapse at the knee, regardless of the cause.
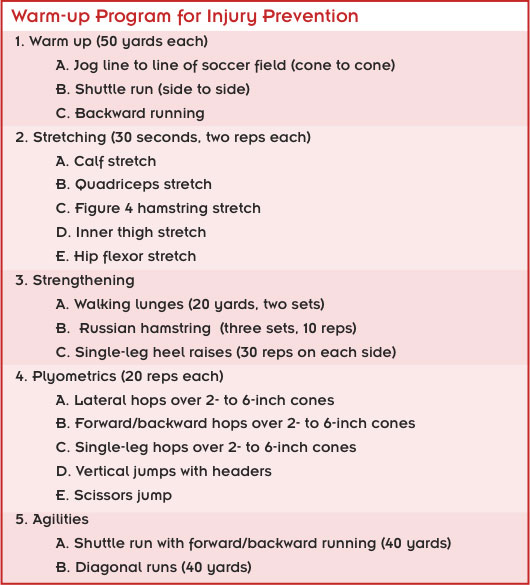
Table 1. Preventive exercises/agility drills as described by Gilchrist et al.[26]
| The low arch in late stance |
Even though excessive pronation associated with a low arch is troublesome during early stance because it overloads the medial foot and is associated with a more rapid rate of calcaneal eversion,[10] excessive pronation during late stance is even more likely to result in foot injury as it drives the head of the talus downward, forcefully separating the sustentaculum tali from the navicular acetabulum. This action increases tensile strain on the plantar calcaneonavicular ligaments (especially the sling ligament) and the plantar fascia, eventually leading to plastic deformity of these important restraining tissues.
An overstretched sling ligament is troublesome as the tibialis posterior muscle is unable to compensate for laxity in this important restraining ligament [29] and the talus is allowed to continue its plantar migration, straining the plantar fascia. Over time, the added tensile strain on the plantar fascia may inhibit the natural tension banding effect associated with the windlass mechanism, eventually leading to collapse of the tarsal bones.
Biomechanically, the most detrimental aspect of excessive talar adduction is that it increases the body’s lever arm for maintaining the subtalar joint in a fully pronated position throughout midstance and propulsion. This has significant effects on both the proximal kinetic chain and the medial forefoot. During midstance, because the adducted talus is held in a fixed position by superimposed body weight, the external rotation moment created by the swing limb is unable to generate a force strong enough to abduct the talus. As a result, the torsional forces associated with this external rotation moment must be temporarily stored in the stance limb. The release of these stored torsional forces is occasionally evidenced by a sudden “abductory twist” of the rearfoot as heel lift occurs; i.e., because ground reaction forces no longer maintain the plantar heel, the entire rearfoot is free to snap medially, as though released from a loaded spring.
Because a chain is most likely to give at its weakest link, the prolonged application of these forces may produce transverse plane laxity of the lower extremity joint capsules, and the knee is most likely to be affected by these torsional forces. Coplan [30] corroborated this by noting that individuals with excessive ranges of subtalar pronation were more likely to display significantly greater ranges of tibiofemoral rotation than normal controls, particularly as the knee approached full extension (its normal position of function as torsional strains peak during late midstance).
In her study, in which participants were tested while non-weightbearing, the mean range of tibial rotation when the knee was flexed 5° was 11.4° for the normal group and 18.5° for the pronating group. She speculated that the opposing rotary torques present during the late midstance period produced laxity in the tissues that normally limit knee rotation. It is also possible, however, that overpronators inherently are more likely to present with ligamentous laxity, which would result in larger ranges of tibiofemoral rotation.
While excessive subtalar pronation during midstance predisposes to injury because of conflicting movement patterns between the leg and talus, continued subtalar pronation through the propulsive period may be even more destructive because it maintains a parallelism of the midtarsal axes. The continued parallelism of these axes essentially unlocks the articulations at a time when maximum stability is needed. This results in a pathological shifting of the tarsal bones as ground reaction forces peak during early propulsion: the foot is forced to behave as a flexible lever arm rather than as the rigid beam necessary to withstand vertical forces.
| Conclusion |
Although early research suggested a limited connection between arch height and lower extremity function, more recent research confirms that arch height does indeed affect function. Information obtained from measurements that accurately identify the height of the medial longitudinal arch may lead to more effective treatment protocols. By identifying specific injuries associated with low and high arches, it may also be possible to prevent these injuries.
| Thomas C. Michaud, DC, published his first book, Foot Orthoses and Other Forms of Conservative Foot Care, in 1993. This article has been excerpted from his new text, Human Locomotion: The Conservative Management of Gait-Related Disorders, which is available at www.humanlocomotion.org. |
Source Lower Extremity Review
| References |
- Effects of arch height of the foot on angular motion of the lower extremities in running, Nigg BM, Cole GK, Nachbauer W. J Biomech 1993;26(8):909-916.
- Measurements used to characterize the foot and the medial longitudinal arch: reliability and validity, Williams DS, McClay IS. Phys Ther 2000;80(9):864-871.
- Arch structure and injury patterns in runners, Williams DS, McClay IS, Hamill J. Clin Biomech 2001;16(4):341-347.
- Development of the child’s arch, Gould N, Moreland M, Alvarez R, Trevino S, Fenwick J. Foot Ankle 1989;9(5):241-245.
- The influence of footwear on the prevalence of flat foot. A survey of 2300 children, Rao UB, Joseph B. J Bone Joint Surg Br 1992;74(4):525-527.
- Running-related injury prevention through barefoot adaptations, Robbins SE, Hanna AM. Med Sci Sports Exerc 1987;19(2):148-156.
- The flat-footed child—To treat or not to treat, what is the clinician to do? Evans A. J Am Podiatr Med Assoc 2008;98(5):383-393.
- Hypermobile flatfoot in children. Comprehension, evaluation and treatment, Bordelon R. Clin Orthop Relat Res 1983;181:7-14.
- Hypermobile flatfoot with short tendo Achilles, Harris RI, Beath T. J Bone Joint Surg Am 1948;30(1):116-138.
- Lower extremity kinematic and kinetic differences in runners with high and low arches, Williams DS, McClay IS, Hamill J, Buchanan TS. J Appl Biomech 2001;17(2):153-163.
- A prospective study of gait related risk factors for exercise-related lower leg pain, Willems TM, De Clercq D, Delbaere K, Vanderstraeten G, De Cock A, Witvrouw E. Gait Posture 2006;23(1):91-98.
- Evaluation of lower extremity overuse injury potential in runners, Hreljac A, Marshall RN, Hume PA. Med Sci Sports Exerc 2000;32(9):1635-1641.
- Etiologic factors associated with selected running injuries, Messier SP, Pittala KA. Med Sci Sports Exerc 1988;20(5):501-505.
- Support phase kinematics of the foot, Scranton PE, Rutkowski R, Brown TD. In The Foot and Ankle,Bateman JE, Trott AW, eds. New York: Thieme-Stratton; 1980.
- An evaluation of the effect of orthotics on force distribution and rearfoot movement during running, Cavanagh PR, Clarke T, Williams K, et al. Presented at the American Orthopaedics Society Sports Medicine Meeting, Lake Placid, NY, June 1978.
- Some biomechanical aspects of the foot and ankle in athletes with and without shin splints, Vtasalo JT, Kvist M. Am J Sports Med 1983;11(3):125-130.
- Stress fractures in athletes. A study of 320 cases, Matheson GO, Clement DB, McKenzie DC, Taunton JE, Lloyd-Smith DR, MacIntyre JG. Am J Sports Med 1987;15(1):46-58.
- Free moment as a predictor of tibial stress fracture in distance runners, Milner CE, Davis IS, Hamill J. J Biomech 2006;39(15):2819-2825.
- Mechanical properties of bone, Riegger C. In: Orthopedic and Sports Physical Therapy, Gould JA, Davies GJ (eds), St. Louis: Mosby; 1985;3-49.
- Foot and ankle characteristics in patellofemoral pain syndrome: a case control study, Barton CJ, Bonanno D, Levinger P, Menz HB. J Orthop Sports Phys Ther 2010;40(5):286-296.
- Foot posture in people with medial compartment knee osteoarthritis, Levinger P1, Menz HB, Fotoohabadi MR, Feller JA, Bartlett JR, Bergman NR. J Foot Ankle Res. 2010 Dec 16;3:29. doi: 10.1186/1757-1146-3-29.
- Foot inversion-eversion and knee kinematics during walking, Lafortune MA, Cavanagh PR, Sommer HJ, Kalenak A. J Orthop Res 1994;12(3):412-420.
- The relationship between static posture and ACL injuries in female athletes, Loudon JK, Jenkins W, Loudon KL. J Orthop Sports Phys Ther 1996;24(2):91-97.
- Sagittal plane biomechanics cannot injure the ACL during sidestep cutting, McLean SG, Huang X, Su A, Van Den Bogert AJ. Clin Biomech (Bristol, Avon). 2004 Oct;19(8):828-38.
- Knee valgus during drop jumps in National Collegiate Athletic Association Division I female athletes. The effect of a medial post, Joseph M, Tiberio D, Baird JL, Trojian TH, Anderson JM, Kraemer WJ, Maresh CM. Am J Sports Med 2008;36(2):285-289.
- A randomized controlled trial to prevent noncontact anterior cruciate ligament injury in female collegiate soccer players, Gilchrist J, Mandelbaum BR, Melancon H, Ryan GW, Silvers HJ, Griffin LY, Watanabe DS, Dick RW, Dvorak J. Am J Sports Med 2008;36(8):1476-1483.
- The effect of neuromuscular training on the incidence of knee injury in female athletes. A prospective study, Hewett TE, Lindenfeld TN, Riccobene JV, Noyes FR. Am J Sports Med 1999;27(6):699-706.
- Effect of neuromuscular warm-up on injuries in female soccer and basketball athletes in urban public high schools: cluster randomized controlled trial, LaBella CR, Huxford MR, Grissom J, Kim KY, Peng J, Christoffel KK. Arch Pediatr Adolesc Med 2011;165(11):1033-1040.
- The effects of sectioning the spring ligament on rearfoot stability and posterior tibial tendon efficiency, Jennings MM, Christensen JC. J Foot Ankle Surg. 2008 May-Jun;47(3):219-24. doi: 10.1053/j.jfas.2008.02.002. Epub 2008 Mar 28.
- Rotational motion of the knee: a comparison of normal and pronating subjects, Coplan JA. J Orthop Sports Phys Ther 1989;10(9):366-369.
- Movements of the subtalar and transverse tarsal joints, Manter JT. Anat. Rec. August 1941. 80: 397–410. doi:10.1002/ar.1090800402
Measurements Used to Characterize the Foot and the Medial Longitudinal Arch: Reliability and Validity, Williams DS, McClay IS. Phys Ther 2000;80(9):864-871.
Poster: The energy return properties of the longitudinal arch in jumping, Saša Čigoja, Michael J. Asmussen, Colin R. Firmingerc, Jared R. Fletcher, W. Brent Edwards, Benno M. Nigg. XXVII Congress of the International Society of Biomechanics and 43rd Annual Meeting of the American Society of Biomechanics. ISB/ASB 2019, Calgary, Canada





