Gait retraining improves symptoms of knee OA
Walking differently to reduce knee pain.
A number of different gait modifications have been demonstrated to significantly reduce the knee adduction moment in patients with knee osteoarthritis (OA). Now research suggests gait retraining can also help reduce the pain associated with knee OA and improve function.

Prague, Czechia. Photo by Stepan Unar on Unsplash
By Pete B. Shull PhD, Lower Extremity Review August 2013
Knee osteoarthritis (OA) affects roughly one in five adults older than 45 years and nearly two in five adults older than 60 years.[1] Among those suffering from symptomatic knee OA, 80% report some degree of movement limitation, 40% self-evaluate their health as either “poor” or “fair,” 25% cannot perform major activities of daily living, and 14% require help with routine tasks.[2] These individuals commonly report difficulty while walking a quarter mile or more, kneeling, stooping, crouching, or climbing stairs.[2]
In addition to the disability and decreased quality of life, knee OA creates a significant financial burden for society and for the individual,[3,4] and the associated medical costs are escalating.[5] At the same time, the incidence rate of knee OA continues to grow due to an aging baby boomer generation, increased life expectancy, and rising rates of obesity.[5]
Though some risk factors for knee OA are non-modifiable, such as age and gender,[7] there are proactive ways to reduce knee joint loading and the associated risk of knee OA progression. While a commonly prescribed and effective way to reduce knee loading is to simply lose weight, recent research has also shown that gait retraining (Figure 1) is a promising conservative treatment for knee OA that can reduce knee loading [8] and alleviate knee pain.[9]
| The problem: uneven knee joint loading |
Knee joint loading has long been linked to knee OA.[10] The medial and lateral compartments of the knee are unevenly loaded during walking gait, with the medial compartment typically absorbing much higher loads than the lateral compartment. This uneven loading phenomenon may at least partially explain why OA is roughly 10 times more likely to affect the medial compartment than the lateral compartment.[11] Medial compartment knee OA leads to articular cartilage loss relative to the healthy cartilage of the lateral compartment (Figure 2), as well as sclerosis and the formation of osteophytes. This can create pain, discomfort, and, eventually, immobility for individuals with the disease.
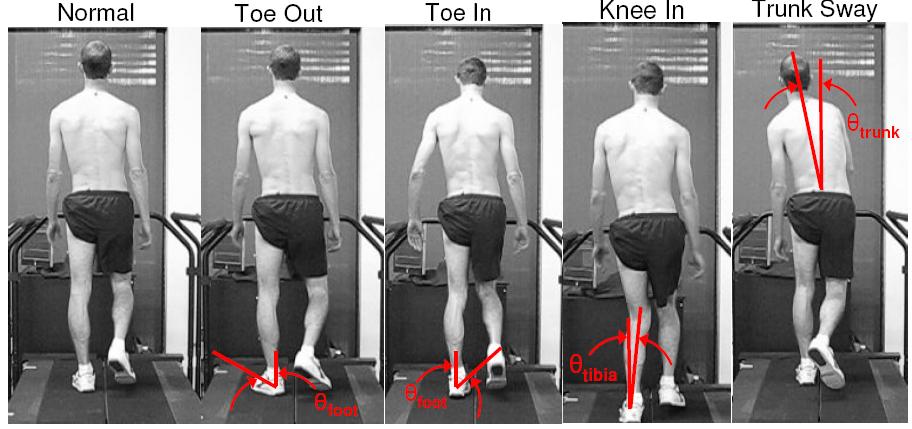
Figure 1: Toe-in gait has been shown to reduce knee pain and improve knee function for individuals with knee osteoarthritis after six weeks of training.[9] Illustration from Gait Retraining, Biomimetics & Dextrous Manipulation Laboratory BDML, Stanford University.
The knee adduction moment (KAM) is a surrogate measure of the unevenness in knee loading.[12] With higher knee adduction moments, the medial compartment absorbs more load, while the lateral compartment absorbs less. The KAM occurs during the stance phase of gait, while the foot is in contact with the ground, and the curve representing the KAM over time typically displays two peaks: a first peak during early stance and a second during late stance. The first peak is the larger of the two and has been linked to medial compartment knee osteoarthritis presence,[13] severity,[14] progression,[15] and pain.[16]
It is possible to reduce KAM by reducing the magnitude of the ground reaction force vector. This is why doctors often recommend that individuals with knee osteoarthritis lose weight. It may also be possible to reduce force magnitude for individuals who walk with abrupt and choppy movements by training them to walk more softly, though this is likely to have a minimal effect.
What can be more effective is to walk in a way that reduces the lever arm between the ground reaction force vector’s line of action and the knee joint center. This manner of reducing KAM could be particularly beneficial for individuals with early stage medial compartment knee osteoarthritis as it shifts loading away from the diseased medial compartment to the healthy lateral compartment of the knee.
| How should I walk? |
Research has shown that several gait modifications reduce KAM in healthy people and in individuals with knee osteoarthritis.[8] Some effective gait modifications include toe-in gait, toe-out gait, increased trunk sway, and knee medialization. These modifications are detailed below.
| Toe-in gait |
Toe-in gait involves internally rotating the foot during stance such that the toes are pointed more inwardly compared to a typical foot progression angle. Toe-in gait has been shown to reduce KAM in healthy individuals.17,18 In a recent study, it has also been shown that a toe-in gait requiring 5° of internal foot rotation reduces the first peak KAM by 13% in individuals with symptomatic medial compartment knee osteoarthritis, and that the same toe-in gait does not increase the knee flexion moment.[19]
In that study, KAM was reduced as the knee joint center shifted medially and the center of pressure shifted laterally,[10] which suggests that, during toe-in gait, individuals move their heel laterally and their toes medially. Additionally, individuals with painful knee osteoarthritis who adopted toe-in gait showed reduced knee pain and improved knee function immediately after six weeks of gait retraining and at one-month follow-up.[9]
These studies were performed for a variety of baseline foot progression angles, so even when participants’ normal gait involved toes that were already pointed straight ahead or slightly inward, training additional internal foot rotation provided the same benefits of reduced medial compartment loading as subjects with more externally rotated foot progression angles.
| Toe-out gait |
Toe-out gait occurs as the foot externally rotates, causing the toes to point more outward compared with a typical foot progression angle. There is a linear relationship between the degree of toeing out and the magnitude of the second peak of the KAM in individuals with knee osteoarthritis, as a greater degree of toe-out is associated with a lower second peak knee adduction moment.[20]
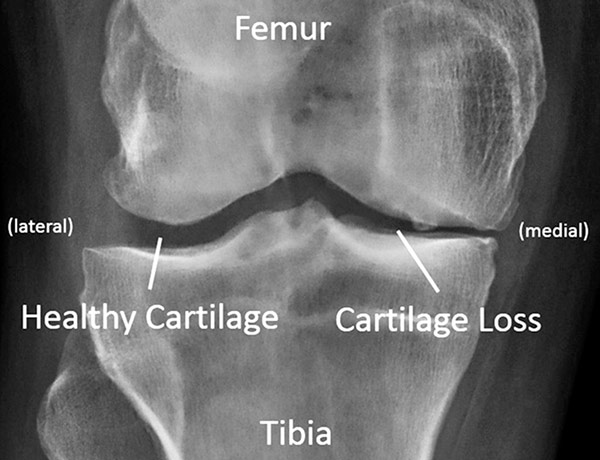
Figure 2: Standing knee x-ray for an individual with medial compartment knee osteoarthritis. The loss of articular cartilage is evident in the narrower gap in the medial compartment.
Additionally, individuals with knee osteoarthritis who learn to toe-out compared with their baseline foot progression angle directly lower the second peak knee adduction moment.[21,22] However, toe-out gait can increase the first peak knee adduction moment.[18] Though toe-out gait reduces the second peak of the knee adduction moment, it is the first peak that has been linked to the presence,[13] severity,[14] and progression [15] of medial compartment knee osteoarthritis and thus may be the more critical peak to lower.
| Increased trunk sway |
Walking with increased trunk sway shifts weight from the upper body laterally towards the knee joint center during the stance phase of gait. The ground reaction force follows the shifting weight and moves the line of action closer to the knee joint center. This results in a shortened lever arm and a reduced knee adduction moment.
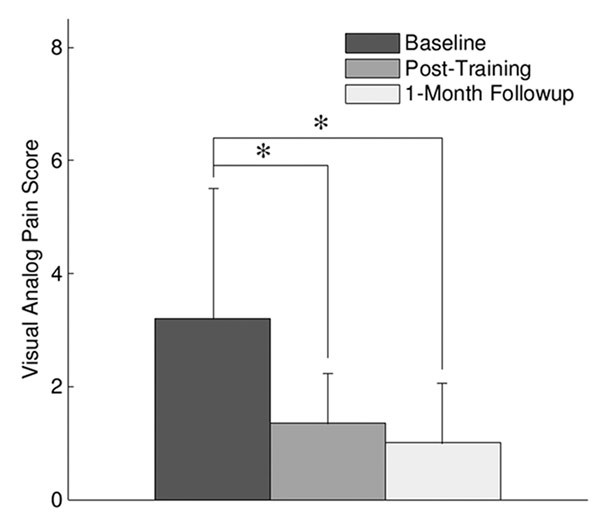
| Figure 3: Reduction in knee pain measured through a visual analog pain scale after six weeks of toe-in gait retraining and at the one-month post-training follow-up.[9] |
Research has shown that the amount of trunk sway is inversely correlated with the magnitude of KAM in patients with knee osteoarthritis.[23] Increased trunk sway has also been suggested as a compensatory strategy to reduce medial compartment loading in patients with severe arthritic symptoms. Greater degrees of trunk sway have been reported in patients with severe knee osteoarthritis compared with patients with mild symptoms.[24] Changing the amount of trunk sway has been shown to reduce both peaks of KAM in healthy individuals.[17,25,26]
However, while increasing trunk sway has been shown to significantly reduce knee adduction moment, there may be some potential drawbacks. It is possible that increasing trunk sway could increase the risk of falling in patients with knee osteoarthritis. Some patients may be less inclined to adopt a gait pattern with increased trunk sway because it appears unnatural. Additionally, individuals with knee osteoarthritis have reported that they prefer not to adopt an increased trunk sway gait because it, “felt uncomfortable, was difficult to maintain, or decreased balance.” [9]
| Knee medialization |
Medializing gait patterns involves a movement of the knee joint center in the medial direction. The knee joint center moves closer to the line of action of the ground reaction force, which shortens the lever arm and reduces the knee adduction moment. Strategies involving medialized gait patterns have been shown to reduce both the first and second peaks of the KAM in healthy individuals and osteoarthritic patients.[17,27,28]
Medializing gait can be less noticeable and may be easier to learn than other altered gait patterns, such as increased trunk sway. One potential drawback is that medializing gait tends to increase the knee flexion angle and knee flexion moment,[27,28] which could increase the overall contact force on the knee—offsetting any force reduction on the medial compartment achieved from a lowered knee adduction moment.[29]
| Walking differently to reduce knee pain |
Given that several gait modifications have been shown to reduce medial compartment knee loading, the question arises: Can walking differently reduce knee pain? Though this question has not yet been explored in depth, a recent study examined how an altered gait pattern can reduce knee pain after six weeks of training.[9]
In this study, 10 individuals with early stage medial compartment knee osteoarthritis and self-reported knee pain performed weekly gait retraining sessions for six weeks. Wearable haptic (touch) devices were used to provide real-time biofeedback [17,30] to train subjects to internally rotate their feet (i.e., adopt a toe-in gait) [19] to reduce the knee adduction moment. Haptic feedback was given with a single vibration motor attached to the lower leg.
A 500-ms vibration pulse on the leg was given during stance to indicate when that toes should be pointed more inwardly, and no vibration indicated that no correction was needed. During each step, kinematics were computed in real-time during the first half of stance and the vibration motor automatically vibrated during the last half of stance when the foot was not internally rotated. Subjects readily understood and quickly adapted to this type of haptic feedback gait training.
Participants performed weekly training sessions to reinforce the new walking pattern and were encouraged to practice on their own at home or at work throughout the week. The standardized Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) questionnaire and a 10-point visual analog pain scale score were measured at baseline, at the end of six weeks of training, and one month after training ended to assess changes in knee pain and knee function.
The results of the study showed that, on average for all participants, gait retraining reduced the first peak of the KAM by 20% as a result of a 7° internal foot rotation (i.e., toe-in gait). WOMAC pain scores improved by 29% post-training, and WOMAC function improved by 32%. The visual analog pain scale score improved by two points, (Figure 3).
Although there wasn’t a specific placebo control group, as with all osteoarthritis interventions, there was an expected placebo effect.[31] However, changes in WOMAC pain and function were approximately 75% larger than the expected placebo effect, which suggests that the improvements were due at least in part to the reduced mechanical loading on the medial compartment of the knee.
Changes in the knee adduction moment, foot progression angle, WOMAC pain and function scores, and visual analog pain score were retained at the follow-up session, one month after the end of the six-week training. The results of this study are promising and show that gait retraining programs for individuals with medial compartment knee osteoarthritis can alleviate knee pain and improve knee function.
| Moving forward |
To make gait retraining a viable treatment option for individuals with medial compartment knee osteoarthritis, longitudinal testing must be performed. The primary question is: does gait retraining ultimately slow knee osteoarthritis progression?
While initial research has been promising in demonstrating that altered gait patterns can not only reduce knee loading but also reduce knee pain and improve function, the long-term outcome of adopting a new walking pattern is unclear. Studies examining six-month, one-year, five-year, and 10-year outcomes of gait retraining would provide deeper insights. Of particular importance is whether gait retraining slows the radiographic progression of knee osteoarthritis compared with no intervention. Also, does pain continue to lessen over time by walking with a new gait pattern or does it revert to pretesting levels?
There is much evidence to suggest a positive long-term outcome, but only time and future research will tell. It is exciting to consider that an act as simple as changing the way one walks could have a profound impact on such a prevalent and debilitating disease.
| Pete B. Shull, PhD, is an assistant professor at the State Key Laboratory of Mechanical System and Vibration, School of Mechanical Engineering, Shanghai Jiao Tong University, in Shanghai, China. |
Source Lower Extremity Review
| Further reading |
Six-week gait retraining program reduces knee adduction moment, reduces pain, and improves function for individuals with medial compartment knee osteoarthritis, Shull PB, Silder A, Shultz R, Dragoo JL, Besier TF, Delp SL, Cutkosky MR. J Orthop Res. 2013 Jul;31(7):1020-5. doi: 10.1002/jor.22340. Epub 2013 Mar 12.
A biomechanical perspective on physical therapy management of knee osteoarthritis, Farrokhi S, Voycheck CA, Tashman S, Fitzgerald GK. J Orthop Sports Phys Ther. 2013 Sep;43(9):600-19. doi: 10.2519/jospt.2013.4121.
| References |
- Estimates of the Prevalence of Arthritis and Other Rheumatic Conditions in the United States, Part II, Reva C. Lawrence MPH, David T. Felson MD MPH, Charles G. Helmick MD, Lesley M. Arnold MD, Hyon Choi MD DrPH, Richard A. Deyo MD MPH, Sherine Gabriel MD MSc, Rosemarie Hirsch MD MPH, Marc C. Hochberg MD MPH, Gene G. Hunder MD, Joanne M. Jordan MD MPH, Jeffrey N. Katz MD, Hilal Maradit Kremers MD MSc, and Frederick Wolfe MD. Arthritis Rheum. 2008 Jan; 58(1): 26–35. doi: 10.1002/art.23176
- Prevalence of knee osteoarthritis in the United States: arthritis data from the Third National Health and Nutrition Examination Survey 1991-94, Dillon CF, Rasch EK, Gu Q, Hirsch R. J Rheumatol. 2006 Nov;33(11):2271-9. Epub 2006 Oct 1.
- Direct medical costs unique to people with arthritis, Gabriel SE, Crowson CS, Campion ME, O’Fallon WM. J Rheumatol. 1997 Apr;24(4):719-25.
- The economic burden associated with osteoarthritis, rheumatoid arthritis, and hypertension: a comparative study, A Maetzel, L Li, J Pencharz, G Tomlinson, and C Bombardier. Ann Rheum Dis. 2004 Apr; 63(4): 395–401. doi: 10.1136/ard.2003.006031
- Medical care expenditures and earnings losses among persons with arthritis and other rheumatic conditions in 2003, and comparisons with 1997, Yelin E, Murphy L, Cisternas MG, Foreman AJ, Pasta DJ, Helmick CG. Arthritis Rheum. 2007 May;56(5):1397-407.
- Osteoarthritis: an overview of the disease and its treatment strategies, Sarzi-Puttini P, Cimmino MA, Scarpa R, Caporali R, Parazzini F, Zaninelli A, Atzeni F, Canesi B. Semin Arthritis Rheum. 2005 Aug;35(1 Suppl 1):1-10.
- Prevalence of knee symptoms and radiographic and symptomatic knee osteoarthritis in African Americans and Caucasians: the Johnston County Osteoarthritis Project, Jordan JM, Helmick CG, Renner JB, Luta G, Dragomir AD, Woodard J, Fang F, Schwartz TA, Abbate LM, Callahan LF, Kalsbeek WD, Hochberg MC. J Rheumatol. 2007 Jan;34(1):172-80.
- Gait modification strategies for altering medial knee joint load: a systematic review, Simic M, Hinman RS, Wrigley TV, Bennell KL, Hunt MA. Arthritis Care Res (Hoboken). 2011 Mar;63(3):405-26. doi: 10.1002/acr.20380. Epub 2010 Oct 27.
- Six-week gait retraining program reduces knee adduction moment, reduces pain, and improves function for individuals with medial compartment knee osteoarthritis, Shull PB, Silder A, Shultz R, Dragoo JL, Besier TF, Delp SL, Cutkosky MR. J Orthop Res. 2013 Jul;31(7):1020-5. doi: 10.1002/jor.22340. Epub 2013 Mar 12.
- Interaction between active and passive knee stabilizers during level walking, Schipplein OD, Andriacchi TP. J Orthop Res. 1991 Jan;9(1):113-9.
- Osteoarthrosis of the knee. A radiographic investigation, Ahlbäck S. Acta Radiol Diagn (Stockh). 1968:Suppl 277:7-72.
- Test-retest reliability of the peak knee adduction moment during walking in patients with medial compartment knee osteoarthritis, Birmingham TB, Hunt MA, Jones IC, Jenkyn TR, Giffin JR. Arthritis Rheum. 2007 Aug 15;57(6):1012-7.
- The knee adduction moment during gait in subjects with knee osteoarthritis is more closely correlated with static alignment than radiographic disease severity, toe out angle and pain, Hurwitz DE, Ryals AB, Case JP, Block JA, Andriacchi TP. J Orthop Res. 2002 Jan;20(1):101-7.
- Knee adduction moment, serum hyaluronan level, and disease severity in medial tibiofemoral osteoarthritis, Sharma L, Hurwitz DE, Thonar EJ, Sum JA, Lenz ME, Dunlop DD, Schnitzer TJ, Kirwan-Mellis G, Andriacchi TP. Arthritis Rheum. 1998 Jul;41(7):1233-40.
- Dynamic load at baseline can predict radiographic disease progression in medial compartment knee osteoarthritis, Miyazaki T, Wada M, Kawahara H, Sato M, Baba H, Shimada S. Ann Rheum Dis. 2002 Jul;61(7):617-22.
- Relationship between pain and medial knee joint loading in mild radiographic knee osteoarthritis, Thorp LE, Sumner DR, Wimmer MA, Block JA. Arthritis Rheum. 2007 Oct 15;57(7):1254-60.
- Training multi-parameter gaits to reduce the knee adduction moment with data-driven models and haptic feedback, Shull PB, Lurie KL, Cutkosky MR, Besier TF. J Biomech. 2011 May 17;44(8):1605-9. doi: 10.1016/j.jbiomech.2011.03.016. Epub 2011 Apr 2.
- The effectiveness of voluntary modifications of gait pattern to reduce the knee adduction moment, van den Noort JC, Schaffers I, Snijders J, Harlaar J. Hum Mov Sci. 2013 Jun;32(3):412-24. doi: 10.1016/j.humov.2012.02.009. Epub 2013 May 4.
- Toe-in gait reduces the first peak knee adduction moment in patients with medial compartment knee osteoarthritis, Shull PB, Shultz R, Silder A, Dragoo JL, Besier TF, Cutkosky MR, Delp SL. J Biomech. 2013 Jan 4;46(1):122-8. doi: 10.1016/j.jbiomech.2012.10.019. Epub 2012 Nov 10.
- Lower limb alignment and foot angle are related to stance phase knee adduction in normal subjects: a critical analysis of the reliability of gait analysis data, Andrews M, Noyes FR, Hewett TE, Andriacchi TP. J Orthop Res. 1996 Mar;14(2):289-95.
- The influence of foot progression angle on the knee adduction moment during walking and stair climbing in pain free individuals with knee osteoarthritis, Guo M, Axe MJ, Manal K. Gait Posture. 2007 Sep;26(3):436-41. Epub 2006 Nov 28.
- Effect of foot rotation on knee kinetics and hamstring activation in older adults with and without signs of knee osteoarthritis, Lynn SK, Costigan PA. Clin Biomech (Bristol, Avon). 2008 Jul;23(6):779-86. doi: 10.1016/j.clinbiomech.2008.01.012. Epub 2008 Mar 14.
- Lateral trunk lean explains variation in dynamic knee joint load in patients with medial compartment knee osteoarthritis, Hunt MA, Birmingham TB, Bryant D, Jones I, Giffin JR, Jenkyn TR, Vandervoort AA. Osteoarthritis Cartilage. 2008 May;16(5):591-9. doi: 10.1016/j.joca.2007.10.017. Epub 2008 Feb 21.
- Individuals with severe knee osteoarthritis (OA) exhibit altered proximal walking mechanics compared with individuals with less severe OA and those without knee pain, Hunt MA, Wrigley TV, Hinman RS, Bennell KL. Arthritis Care Res (Hoboken). 2010 Oct;62(10):1426-32. doi: 10.1002/acr.20248.
- Implications of increased medio-lateral trunk sway for ambulatory mechanics, Mündermann A, Asay JL, Mündermann L, Andriacchi TP. J Biomech. 2008;41(1):165-70. Epub 2007 Aug 3.
- Feasibility of a gait retraining strategy for reducing knee joint loading: increased trunk lean guided by real-time biofeedback, Hunt MA, Simic M, Hinman RS, Bennell KL, Wrigley TV. J Biomech. 2011 Mar 15;44(5):943-7. doi: 10.1016/j.jbiomech.2010.11.027. Epub 2010 Dec 7.
- Gait retraining to reduce the knee adduction moment through real-time visual feedback of dynamic knee alignment, Barrios JA, Crossley KM, Davis IS. J Biomech. 2010 Aug 10; 43(11): 2208–2213. Published online 2010 May 8. doi: 10.1016/j.jbiomech.2010.03.040
- Design of Patient-Specific Gait Modifications for Knee Osteoarthritis Rehabilitation, Benjamin J. Fregly, Jeffrey A. Reinbolt, Kelly L. Rooney, Kim H. Mitchell, and Terese L. Chmielewski. IEEE Trans Biomed Eng. 2007 Sep; 54(9): 1687–1695. doi: 10.1109/TBME.2007.891934
- Decreased knee adduction moment does not guarantee decreased medial contact force during gait, Walter JP, D’Lima DD, Colwell CW Jr, Fregly BJ. J Orthop Res. 2010 Oct;28(10):1348-54. doi: 10.1002/jor.21142.
- Real-time knee adduction moment feedback for gait retraining through visual and tactile displays, Wheeler JW, Shull PB, Besier TF. J Biomech Eng. 2011 Apr;133(4):041007. doi: 10.1115/1.4003621.
- The placebo effect and its determinants in osteoarthritis: meta-analysis of randomised controlled trials, Zhang W, Robertson J, Jones AC, Dieppe PA, Doherty M. Ann Rheum Dis. 2008 Dec;67(12):1716-23. doi: 10.1136/ard.2008.092015. Epub 2008 Jun 9.
Also see
Gait Retraining Biomimetics & Dextrous Manipulation Laboratory, Stanford University
On the move: Gait training improves limited mobility Lower Extremity Review