UCalgary scientists discover a new way to battle multiple sclerosis
Findings challenge conventional thinking about the root cause of MS.
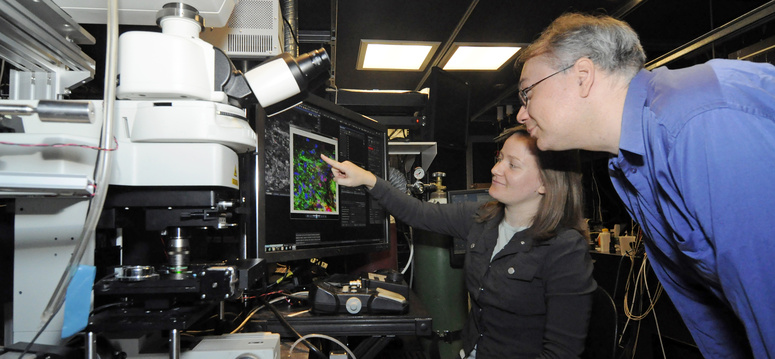
The Dr. Peter Stys lab within the Hotchkiss Brain Institute at the Cumming School of Medicine, University of Calgary, is equipped with highly specialized microscopes used for researching multiple sclerosis, Alzheimer’s and other neurodegenerative disease. Researchers can’t wear white lab coats, they have to wear dark clothing. Photons could reflect off light clothing and interfere with the experiments. From left: Megan Morgan, research assistant, and Craig Brideau, engineering scientist. Pauline Zulueta, Cumming School of Medicine.
By Kelly Johnston, Cumming School of Medicine, University of Calgary May 7, 2018
Ridiculous. That’s how Andrew Caprariello says his colleagues described his theory about multiple sclerosis (MS) back when he was doing his PhD in Ohio.
Caprariello’s passion to explore controversial new theories about MS propelled him to seek out a postdoctoral fellowship with a like-minded thinker, whom he found in University of Calgary’s Dr. Peter Stys, a member of the Hotchkiss Brain Institute at the Cumming School of Medicine (CSM).
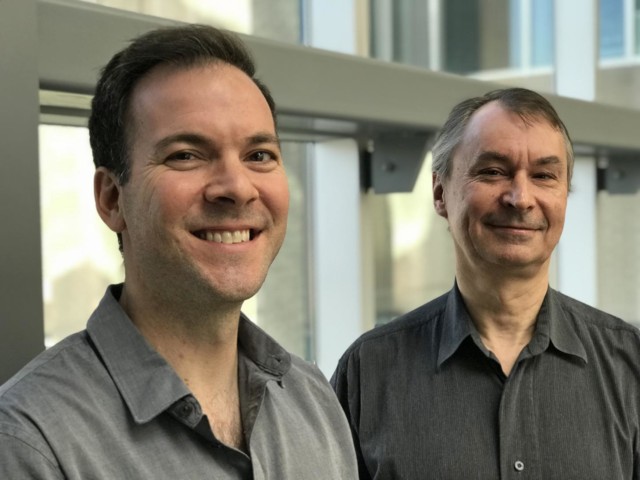
University of Calgary scientists Andrew Caprariello PhD, left, and Dr. Peter Stys, professor at the Cumming School of Medicine, are challenging conventional thinking about the root cause of multiple sclerosis. Cumming School of Medicine
The collaboration paid off. Caprariello, Stys and their colleagues have scientific proof published in the Proceedings of the National Academy of Sciences (PNAS) that their somewhat radical theory has merit. “I’ve always wondered what if MS starts in the brain and the immune attacks are a consequence of the brain damage,” says Caprariello, PhD, and lead author on the study.
Currently, MS is considered to be a progressive autoimmune disease. Brain inflammation happens when the body’s immune system attacks a protective material around nerve fibers in the brain called myelin. Conventional thinking is that rogue immune cells initially enter the brain and cause myelin damage that starts MS.
“In the field, the controversy about what starts MS has been brewing for more than a decade. In medical school, I was taught years ago that the immune attack initiates the disease. End of story,” says Stys, a neurologist and professor in the Department of Clinical Neurosciences at the CSM. “However, our findings show there may be something happening deeper and earlier that damages the myelin and then later triggers the immune attacks.”
To test the theory, the research team designed a mouse model of MS that begins with a mild myelin injury. In this way, researchers could mirror what they believe to be the earliest stages of the disease.
“Our experiments show, at least in this animal model, that a subtle early biochemical injury to myelin secondarily triggers an immune response that leads to additional damage due to inflammation. It looks very much like an MS plaque on MRI and tissue examination,” says Stys. “This does not prove that human MS advances in the same way, but provides compelling evidence that MS could also begin this way.”
With that result, the researchers started to investigate treatments to stop the degeneration of the myelin to see if that could reduce, or stop, the secondary autoimmune response.
“We collaborated with researchers at the University of Toronto and found that by targeting a treatment that would protect the myelin to stop the deterioration, the immune attack stopped and the inflammation in the brain never occurred,” says Stys. “This research opens a whole new line of thinking about this disease. Most of the science and treatment for MS has been targeted at the immune system, and while anti-inflammatory medications can be very effective, they have very limited benefit in the later progressive stages of the disease when most disability happens.”
It can be very hard to find funding to investigate an unconventional theory. The research team was funded by the Brain and Mental Health Strategic Research Fund, established by the Office of the Vice-President (Research) at UCalgary to support innovative, interdisciplinary studies within the Brain and Mental Health research strategy.
“We chose high-risk, novel projects for these funds to support discoveries by teams who did not have the chance to work together through conventional funding sources,” said Ed McCauley, PhD, vice-president (research). “The MS study shows the potential of brain and mental health scholars to expand capacity by tapping into new approaches for conducting research. Their work also exemplifies the type of interdisciplinary research that is propelling the University of Calgary as an international leader in brain and mental health research.”
The MS study was one of four interdisciplinary projects awarded funds.
| Led by the Hotchkiss Brain Institute, Brain and Mental Health is one of six research strategies guiding the University of Calgary towards its Eyes High goals. The strategy provides a unifying direction for brain and mental health research at the university and positions researchers to unlock new discoveries and treatments for brain health in our community. |
 Source University of Calgary
Source University of Calgary
| References |
Biochemically altered myelin triggers autoimmune demyelination, Andrew V Caprariello, James A Rogers, Megan L Morgan, Vahid Hoghooghi, Jason R Plemel, Adam Koebel, Shigeki Tsutsui, Jeffrey F Dunn, Lakshmi P Kotra, Shalina S Ousman, V Wee Yong, and Peter K Stys. Proceedings of the National Academy of Sciences PNAS May 2018, 201721115; DOI: 10.1073/pnas.1721115115
Also see
Cumming researchers develop new method to discover drugs to treat epilepsy University of Calgary