Foot rotation during gait in patients with knee OA
Rotating the foot in or out during gait is associated with significant decreases in frontal plane knee load during early or late stance, respectively, and can be effective for reducing pain and potentially slowing the progression of disease in patients with knee osteoarthritis.

Why do I toe out when I run? Run Smart Online
By Kevin Alan Valenzuela ABD CSCS and Hunter Jared Bennett PhD, Lower Extremity Review August 2016
Knee osteoarthritis (OA) has become an increasingly common musculoskeletal diagnosis in the US. Projections suggest that by the year 2030, approximately 25% of the US population will have knee OA.
As knee OA progresses to the end stage of the continuum, a total knee replacement is often the final treatment option. However, nonsurgical means of slowing the progression of knee OA can help to prolong or avoid the costly, invasive, and painful surgery.
| Determinants of knee OA |
It’s been suggested that knee OA occurs as a result of many years of applied force, or loading, to the knee joint. This can happen through uneven force distribution within the joint compartments or movement at the joint to which the individual is unaccustomed; either can lead to excessive cartilage degeneration.
The medial tibiofemoral compartment tends to be the most common site for OA occurrence, with an incidence ratio of 5:1 relative to the lateral compartment. Medial knee OA is often linked to two biomechanical factors: an elevated external knee adduction moment (or internal knee abduction moment; KAM) during the stance phase of gait (Figure 1), and the occurrence of frontal plane shear force medial to the knee joint center during stance phase (Figure 2). Both variables affect loading on individual compartments of the knee joint.
A toeing-out intervention predominantly affects knee loads late in the stance phase of gait, while a toeing-in gait intervention typically affects knee loads in early stance.
The KAM has been prospectively linked to development and progression of medial compartment knee OA. As the KAM value increases, loading on the medial compartment of the knee joint increases, increasing wear on the cartilage. Research has shown individuals with medial knee OA have higher KAM values late in the gait cycle than asymptomatic healthy controls. In vitro studies have found knee joint cartilage deteriorates at a faster rate under shear stress than under pure compressive loading, and this shear stress is also linked to development and progression of knee OA. Medially directed shear force causes wear on the medial compartment, making it an important component to control or minimize in patients with evidence of medial knee OA.
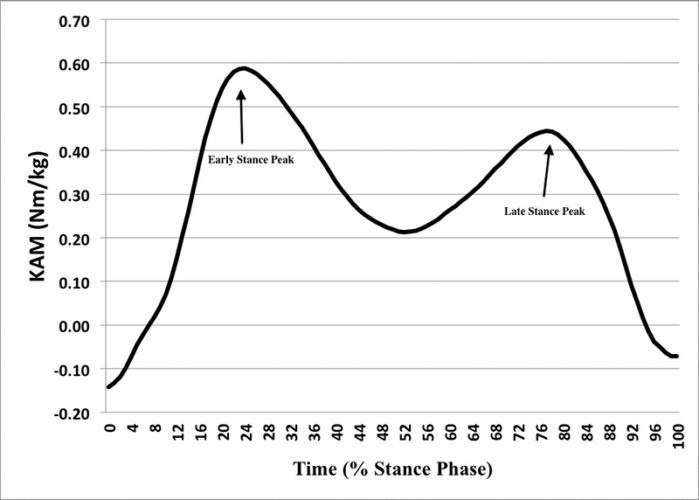
| Figure 1. Stance phase external knee adduction moment over time. |
| Foot rotation interventions |
Interventions, many of which are noninvasive, have been shown to slow the progression of knee OA based on the aforementioned variables. Several laboratory-based investigations have examined foot rotation, tibial inclination angles, lateral trunk sway, and altered step widths as potential ways to slow the progression of knee OA by addressing associated biomechanical variables.
Foot rotation interventions are some of the more commonly studied and used methods of attempting to slow knee OA progression. One reason is the natural occurrence for people in general of foot rotation during gait. Foot rotation is seen as a natural compensatory mechanism to help alleviate pain and slow disease progression. Individuals with medial knee OA have been shown to rotate their feet externally during gait as a means of unloading the affected compartment, which has led to investigations of both external and internal foot rotation interventions. This rotation may offload the medial compartment by reducing KAM and lateral-medial shear force.
As activities increase in complexity and physical demand (stair climbing vs walking, for example), associated joint moments and forces tend to increase, potentially leading to further cartilage degeneration in patients with knee OA.
With the onset of painful knee OA, individuals may bypass certain activities as a means of avoiding pain. This can adversely affect quality of life in these individuals; those who enjoyed hiking with loved ones miss those experiences, for example, while others may choose to restrict their living space if negotiating stairs is too painful to access floors of their home. Similar experiences may occur in individuals who do not have pain; if they have been advised that certain movements put their cartilage at risk, they may proactively compensate to avoid the potential future pain.
Reduced activity levels can have additional consequences, such as weight gain, increased cholesterol, and other adverse physiological effects. Issues such as weight gain can make OA worse, as it places increased force onto already damaged cartilage, likely speeding up the wearing away of remaining tissue.
Ultimately, the best clinical option is an intervention that allows for continued activity (and thus maintenance or improvement of quality of life, depending on the presence of pain or discomfort) while reducing wear on the cartilage. This strategy can delay an end-stage knee OA diagnosis and the need for a total knee replacement.
| Mechanics of foot rotation |
Loading of the medial or lateral tibiofemoral compartments of the knee joint is a product of both the frontal plane position of the knee joint in relation to the center of pressure of the foot, the varus/valgus or abduction/adduction orientation of the knee, and the weight/ force applied to the knee joint. Research has found increased frontal plane knee loads in individuals with medial knee OA are associated with greater varus/adduction of the knee during walking, and not greater external forces. Researchers have investigated the effects of gait modifications such as changes in the foot rotation angle on frontal plane knee loads. Changing foot rotation angle can align the knee center in a more neutral position, reducing the frontal plane moment arm, which should in turn reduce abnormal knee loads. Foot rotation gait modifications also have been associated with reduced pain in people with medial knee OA.
Two different foot rotation gait strategies exist to combat abnormal knee loading: increasing either the toe-out angle or toe-in angle. Both foot rotation modifications are made in relation to the forward progression of the body. While both foot rotation strategies can reduce frontal plane knee loads, each stra2tegy affects knee loading at a different time point during the stance phase of gait. Toeing-out predominantly affects knee loads in late stance, while toeing-in affects knee loads during early stance. Because it is not possible to combine both gait strategies during stance phase, it is important to examine the effects of each strategy independently and discern which is most effective for a given patient or population.
Changing foot rotation angle can align the knee center in a more neutral position, reducing the frontal plane moment arm, which should reduce abnormal knee loads.
| Toeing-out |
An increased toe-out gait is commonly seen in the knee OA population, possibly as an adaptation to medial knee loading. Experimentally, increased toeing-out has been associated with reduced knee loading in the latter half of stance during level walking, running, and stair ascent in both healthy and knee OA populations. Within the current literature, toe-out gait modification studies have assessed foot progression angles of 10°, 20°, 30°, and 40° in both healthy individuals and those with knee OA. In general, the reductions in late stance knee loads seen during level walking increase progressively with increasing toe-out angles.
Similar effects are associated with self-selected toe-out gait in patients with knee OA. Increasing foot angles beyond a self-selected degree of toe-out further reduces frontal plane knee loading and lateral-medial shear force. There is likely a point of diminishing returns, however. Certain toe-out angles would seem to be impractical (90°, for example) and unlikely to be maintainable for any significant time. The idea is to find the maximum benefit, which the individual who already rotates their foot may or may not have found, depending on their chosen level of rotation.
Additional reported advantages of toe-out gait include reducing the summed overall stance phase frontal plane knee loading by 5%, and late-stance medial-lateral shear force by 27%. During level running in healthy individuals, increasing toe-out foot progression angle by 14° is associated with a 6% reduction in peak frontal plane knee loading. Using a 20° toe-out strategy has been used successfully to reduce late stance frontal plane knee loads during stair ascent, but had no effect during stair descent.
Although toe-out has been quite successful in reducing knee loads during late stance, an adverse effect has been observed earlier in stance. Reductions of late stance knee loads associated with increased toe-out angle have been accompanied by increases in early stance phase frontal plane knee loading in some studies, though not all. Early stance phase knee loads are generally larger in magnitude than those associated with late stance, and have garnered much attention. Therefore, increased toe-out gait strategies may be a viable option for individuals with increased frontal plane knee loads during the latter half of stance, but should be monitored for their effects on loading during early stance.
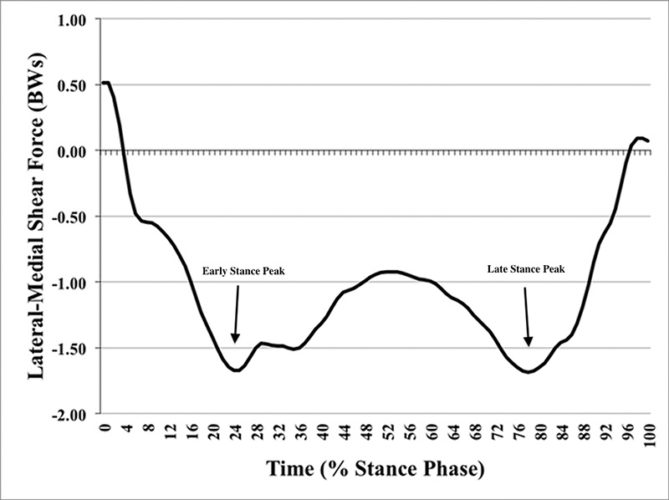
| Figure 2. Stance phase frontal plane shear force over time. |
| Toeing-in |
Increasing toe-in angle has been associated with significantly reduced early stance phase frontal plane knee load during level walking, stair ascent, and level running tasks. Early stance frontal plane knee loading is an important aspect of walking gait, as it is strongly related to both the onset and progression of knee OA.
Experimental toe-in angles have ranged from 5° to 10° (relative to neutral), as well as “maximum comfortable” internal rotation. When instructed to comfortably internally rotate the foot during level running, healthy participants reduced foot rotation angles from their natural alignment of about 11° of toe-out to a more neutral foot progression angle (0°). The change in foot angle during running was associated with a 9% reduction in frontal plane knee loading.
During level walking, toe-in interventions have been associated with reductions of early stance frontal plane knee loading from 13% up to 45%. In further support of toe-in gait, 10° toe-in angles have been associated with reductions in both the early stance knee load and the summed overall stance phase frontal plane knee load in healthy people with varus, valgus, and neutral knee alignments during both level ground and stair ascent tasks. As medial knee OA is most prevalent in individuals with a varus knee malalignment, a toe-in gait may be a particularly important strategy for reducing early stance frontal plane knee loading in those individuals.
The effect of increased toe-in angles on late stance frontal plane knee loads is unclear. Although some studies have found no changes in late stance knee loads using toe-in gait, others found significant increases in late stance loads. Therefore, while toe-in gait can be highly effective in reducing early stance phase knee loads, the potential late-stance effect should be considered before implementing a toe-in gait strategy in individuals who may also have abnormal late stance knee loads.
An interesting result of both toe-out and toe-in gait modifications is the apparent transfer of frontal plane knee loads to the sagittal plane. Several studies have found increases in peak early stance internal knee extension loads associated with both toe-out and toe-in interventions during level walking. However, one study found that a toe-out gait was associated with lower peak knee extension moments than normal walking. Knee off-loading in the sagittal plane has been postulated as a mechanism to reduce compression loads and pain in individuals with knee OA; therefore, increases in sagittal plane loads using modified foot progression angles could increase pain in some individuals. Due to the possibility of load transfer from the frontal plane to the sagittal plane, toe-out and toe-in gait strategies should be monitored for increasing knee loads in other planes.
| Clinical implications |
Ultimately, in choosing whether to use foot rotation as a treatment intervention, practitioners must evaluate individual patient’s goals. As discussed, sometimes the first loading peak is reduced and sometimes the second peak is reduced, depending on the intervention chosen. Each individual’s movement profile should be evaluated whenever possible to determine which peak is likely to be most detrimental.
A thorough analysis (including motion analysis) is ideal, but in reality is not always an option for clinicians. If a high-tech movement analysis system is unavailable, it may be a matter of trial and error with the different rotational interventions to see which one decreases pain and allows for increased movement. It should be noted, however, that a decrease in pain is not always associated with a change in mechanics and therefore does not necessarily indicate a slowing of knee OA progression.
It may look and feel odd at first, but walking “like a duck” may have long-term benefits for slowing knee OA progression, and thus delaying a potential need for a total knee replacement.
| Kevin Alan Valenzuela ABD CSCS, is a PhD student at the University of Tennessee, Knoxville, with a background in clinical and sport biomechanics. Hunter Jared Bennett PhD, is an assistant professor of human movement sciences at Old Dominion University in Norfolk VA, with a background in clinical and sport biomechanics. |
Source Lower Extremity Review
| References |
- Projections of US prevalence of arthritis and associated activity limitations, Hootman JM, Helmick CG. Arthritis Rheum. 2006 Jan;54(1):226-9. Full text
- The effect of internal and external foot rotation on the adduction moment and lateral-medial shear force at the knee during gait, Lynn SK, Kajaks T, Costigan PA. J Sci Med Sport. 2008 Sep;11(5):444-51. Epub 2007 Sep 4.
- High prevalence of lateral knee osteoarthritis in Beijing Chinese compared with Framingham Caucasian subjects, Felson DT, Nevitt MC, Zhang Y, Aliabadi P, Baumer B, Gale D, Li W, Yu W, Xu L. Arthritis Rheum. 2002 May;46(5):1217-22. Full text
- The influence of gait pattern on signs of knee osteoarthritis in older adults over a 5-11 year follow-up period: a case study analysis, Lynn SK, Reid SM, Costigan PA. Knee. 2007 Jan;14(1):22-8. Epub 2006 Nov 7.
- Dynamic load at baseline can predict radiographic disease progression in medial compartment knee osteoarthritis, Miyazaki T, Wada M, Kawahara H, Sato M, Baba H, Shimada S. Ann Rheum Dis. 2002 Jul;61(7):617-22. Full text
- Effect of foot rotation on knee kinetics and hamstring activation in older adults with and without signs of knee osteoarthritis, Lynn SK, Costigan PA. Clin Biomech (Bristol, Avon). 2008 Jul;23(6):779-86. doi: 10.1016/j.clinbiomech.2008.01.012. Epub 2008 Mar 14.
- Does increasing step width alter knee biomechanics in medial compartment knee osteoarthritis patients during stair descent? Paquette MR, Zhang S, Milner CE, Klipple G. Knee. 2014 Jun;21(3):676-82. doi: 10.1016/j.knee.2014.02.020. Epub 2014 Mar 1.
- Toe-in gait reduces the first peak knee adduction moment in patients with medial compartment knee osteoarthritis, Shull PB, Shultz R, Silder A, Dragoo JL, Besier TF, Cutkosky MR, Delp SL. J Biomech. 2013 Jan 4;46(1):122-8. doi: 10.1016/j.jbiomech.2012.10.019. Epub 2012 Nov 10.
- The influence of walking mechanics and time on the results of proximal tibial osteotomy, Wang JW, Kuo KN, Andriacchi TP, Galante JO. J Bone Joint Surg Am. 1990 Jul;72(6):905-9.
- Foot rotation-a potential target to modify the knee adduction moment, Teichtahl AJ, Morris ME, Wluka AE, Baker R, Wolfe R, Davis SR, Cicuttini FM. J Sci Med Sport. 2006 May;9(1-2):67-71. Epub 2006 Apr 19.
- Associations among knee adduction moment, frontal plane ground reaction force, and lever arm during walking in patients with knee osteoarthritis, Hunt MA, Birmingham TB, Giffin JR, Jenkyn TR. J Biomech. 2006;39(12):2213-20. Epub 2005 Oct 5.
- Training multi-parameter gaits to reduce the knee adduction moment with data-driven models and haptic feedback, Shull PB, Lurie KL, Cutkosky MR, Besier TF. J Biomech. 2011 May 17;44(8):1605-9. doi: 10.1016/j.jbiomech.2011.03.016. Epub 2011 Apr 2.
- The influence of foot progression angle on the knee adduction moment during walking and stair climbing in pain free individuals with knee osteoarthritis, Guo M, Axe MJ, Manal K. Gait Posture. 2007 Sep;26(3):436-41. Epub 2006 Nov 28.
- Relationship between gait and clinical results after high tibial osteotomy, Wada M, Imura S, Nagatani K, Baba H, Shimada S, Sasaki S. Clin Orthop Relat Res. 1998 Sep;(354):180-8.
- The knee adduction moment during gait in subjects with knee osteoarthritis is more closely correlated with static alignment than radiographic disease severity, toe out angle and pain, Hurwitz DE, Ryals AB, Case JP, Block JA, Andriacchi TP. J Orthop Res. 2002 Jan;20(1):101-7. PDF
- Altering foot progression angle in people with medial knee osteoarthritis: the effects of varying toe-in and toe-out angles are mediated by pain and malalignment, Simic M, Wrigley TV, Hinman RS, Hunt MA, Bennell KL. Osteoarthritis Cartilage. 2013 Sep;21(9):1272-80. doi: 10.1016/j.joca.2013.06.001. Full text
- The effectiveness of voluntary modifications of gait pattern to reduce the knee adduction moment, van den Noort JC, Schaffers I, Snijders J, Harlaar J. Hum Mov Sci. 2013 Jun;32(3):412-24. doi: 10.1016/j.humov.2012.02.009. Epub 2013 May 4.
- Acute Effects of Foot Rotation in Healthy Adults during Running on Knee Moments and Lateral-Medial Shear Force, Valenzuela KA, Lynn SK, Noffal GJ, Brown LE. J Sports Sci Med. 2016 Feb 23;15(1):50-6. eCollection 2016 Mar. Full text
- Toe-out gait in patients with knee osteoarthritis partially transforms external knee adduction moment into flexion moment during early stance phase of gait: a tri-planar kinetic mechanism, Jenkyn TR, Hunt MA, Jones IC, Giffin JR, Birmingham TB. J Biomech. 2008;41(2):276-83. Epub 2007 Dec 3.
- Static frontal plane tibiofemoral alignments and their effects on knee biomechanics during level walking and stair ascent tasks, Bennett HJ. PhD diss. University of Tennessee, 2016
- The role of varus and valgus alignment in knee osteoarthritis, Sharma L. Arthritis Rheum. 2007 Apr;56(4):1044-7. No abstract available. Full text
- The role of knee alignment in disease progression and functional decline in knee osteoarthritis, Sharma L, Song J, Felson DT, Cahue S, Shamiyeh E, Dunlop DD. JAMA. 2001 Jul 11;286(2):188-95. Erratum in: JAMA 2001 Aug 15;286(7):792.
- Knee adduction moment, serum hyaluronan level, and disease severity in medial tibiofemoral osteoarthritis, Sharma L, Hurwitz DE, Thonar EJ, Sum JA, Lenz ME, Dunlop DD, Schnitzer TJ, Kirwan-Mellis G, Andriacchi TP. Arthritis Rheum. 1998 Jul;41(7):1233-40.
- Simultaneous prediction of muscle and contact forces in the knee during gait, Lin YC, Walter JP, Banks SA, Pandy MG, Fregly BJ. J Biomech. 2010 Mar 22;43(5):945-52. doi: 10.1016/j.jbiomech.2009.10.048. Epub 2009 Dec 5.
- Gait characteristics of patients with knee osteoarthritis, Kaufman KR, Hughes C, Morrey BF, Morrey M, An KN. J Biomech. 2001 Jul;34(7):907-15.
- Weight loss reduces knee-joint loads in overweight and obese older adults with knee osteoarthritis, Messier SP, Gutekunst DJ, Davis C, DeVita P. Arthritis Rheum. 2005 Jul;52(7):2026-32. Full text
Why Do I Toe Out When I Run? in Run Smart Online
